CollaborateMD's Combine Claims feature allows users to merge two or more separate claims into one, consolidating all charges and removing the duplicate claims automatically. This is useful for customers who need to combine encounters into a single claim due to the EHR separating the encounter into multiple claims, payer bundling requirements, or any other reason.
Follow the steps below to combine claims.
-
Select Claim > Claim Control.
-
Enter your Search Criteria or Load a Search Filter.
-
Use the Claim Status drop-down menu to filter by the status of the claim (e.g., Send to insurance via clearinghouse, Balance due patient, User print and mail to insurance, etc.)
-
Place a check in the “Include Deleted” box to include deleted statuses in your search results.
-
Use the Entered Date field to filter the search by the date the claim was entered into CollaborateMD.
-
Use the Date of Service field to filter the search by the date of service on the claim.
-
Use the Last Submitted Date field to filter the search by the date the claim was last submitted.
-
Use the Review Status drop-down menu to filter the search by the review status of the claim (e.g., Unreviewed, Reviewed - Error, etc.).
-
Use the Claim Type drop-down menu to filter the search by Professional, Institutional, or All claims.
-
Use the Current Payer drop-down menu to filter the search by the payer on the claim.
-
Use the Current Payer ID field to filter the search by the Payer ID.
-
Use the Current Payer Type drop-down menu to filter the search by the payer type (e.g., Self-Pay, Medicare, BCBS, etc.).
 You are able to select multiple payer types at once.
You are able to select multiple payer types at once. -
Use the Patient field to filter the search by the exact patient the claim is associated with.
-
Use the Rendering Provider field to filter the search by the rendering provider on the claim.
-
Use the Facilities field to filter the search by the facility on the claim.
-
Use the Procedure Code field to filter the search by procedure code on the claim. Note: You can only search by one procedure code at a time.
 You can use the Customize link to add Practice, Office, Billing Provider, Referring Provider, Supervising/Operating Provider, and Ordering /Other Provider to your Claim Search Options. To do this, check the corresponding box(es) and click the Save button.
You can use the Customize link to add Practice, Office, Billing Provider, Referring Provider, Supervising/Operating Provider, and Ordering /Other Provider to your Claim Search Options. To do this, check the corresponding box(es) and click the Save button. 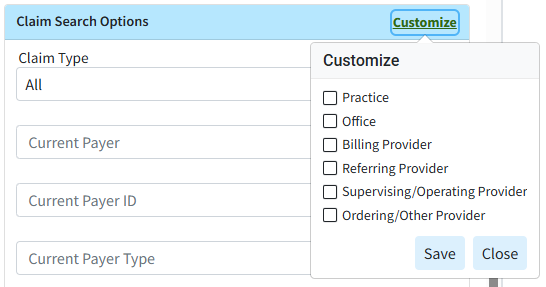
-
Use the Procedure Code field (Under Charge Search Options) to filter the search by procedure code/charge on the claim.
-
Populate the Tracking Status (contains) field to filter the search by keywords in the status message sent back by the payer.
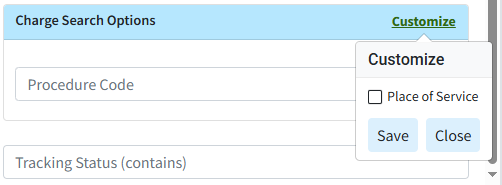
 You can use the Customize link to add Place of Service to your Charge Search Options. To do this, check the corresponding box and click the Save button.
You can use the Customize link to add Place of Service to your Charge Search Options. To do this, check the corresponding box and click the Save button. 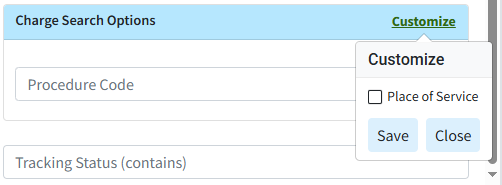
-
-
Click the Search button.
-
Optional: Click on the
 icon to edit your search criteria.
icon to edit your search criteria. Sort your search results. Visit our Reorder Table Columns Help Article for detailed steps on how to hide, rearrange, or add header columns.
Sort your search results. Visit our Reorder Table Columns Help Article for detailed steps on how to hide, rearrange, or add header columns. -
Place a check in the box next to the claims you want to combine.
-
Click the Combine Claims button.
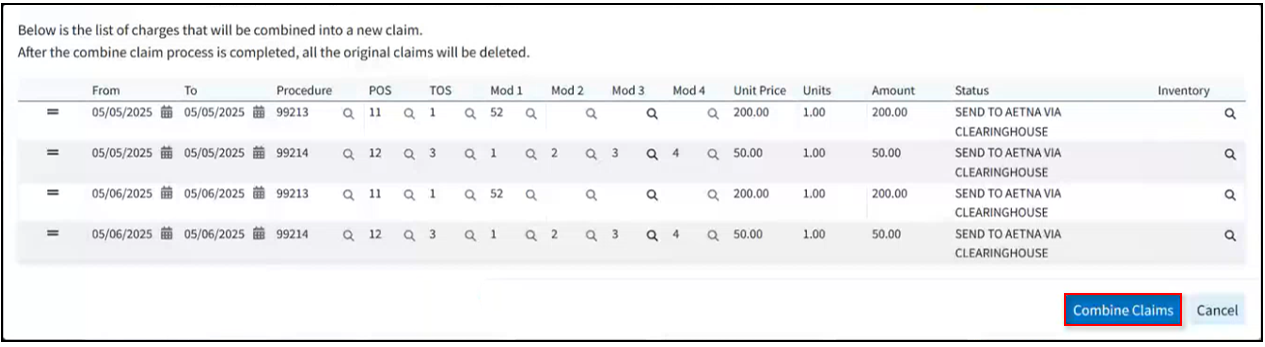
 There is no limitation on the number of claims you choose to combine as long as they are all for the same patient, payer, etc., and the total number of charges combined doesn't exceed the claim charge line limitations (50 for professional and 999 for institutional claims).
There is no limitation on the number of claims you choose to combine as long as they are all for the same patient, payer, etc., and the total number of charges combined doesn't exceed the claim charge line limitations (50 for professional and 999 for institutional claims). -
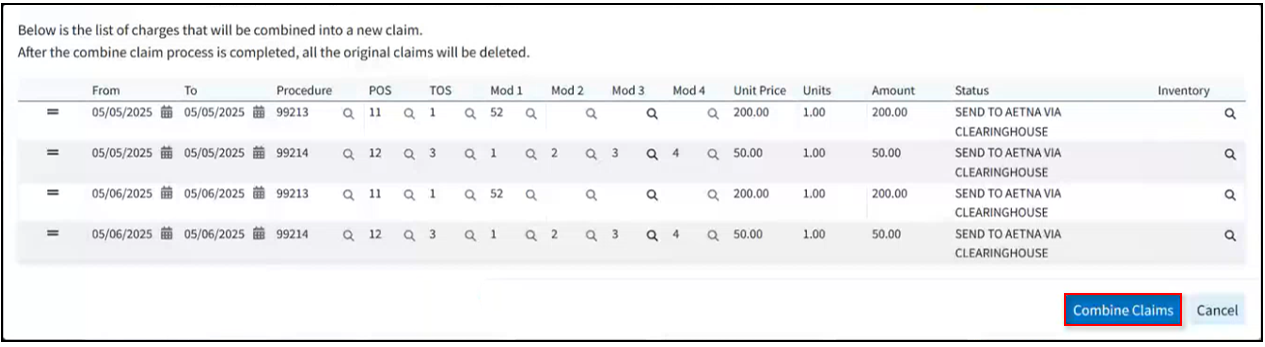
You will be presented with a list of charges that will be combined into the new claim.
- Edit or Reorder charges as needed.
-
Click Combine Claims.
-
A new claim will open. Make any optional updates (additional charges, additional info, ambulance info).
 Please note that at this point, you are not done yet. Until you save this new claim, the existing claims will still exist. Once saved, only the new combined claim will exist, and the individual ones will be deleted.
Please note that at this point, you are not done yet. Until you save this new claim, the existing claims will still exist. Once saved, only the new combined claim will exist, and the individual ones will be deleted.
- Click Save.
 You are able to select multiple payer types at once.
You are able to select multiple payer types at once. You can use the Customize link to add Practice, Office, Billing Provider, Referring Provider, Supervising/Operating Provider, and Ordering /Other Provider to your Claim Search Options. To do this, check the corresponding box(es) and click the Save button.
You can use the Customize link to add Practice, Office, Billing Provider, Referring Provider, Supervising/Operating Provider, and Ordering /Other Provider to your Claim Search Options. To do this, check the corresponding box(es) and click the Save button. 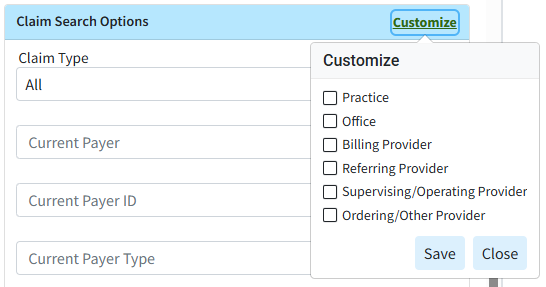
 Sort your search results. Visit our
Sort your search results. Visit our