Highlights
| New Features | Enhancements |
|---|---|
| New Task Assignment to Contact Groups
New Prior Auth Requirement & Billing Alerts Update New Appointment Types Default Codes |
New Taxonomy Specialty Report Fields |
New features
New Task Assignment to Contact Groups
Capitalizing on our recently released Shared Contact Groups feature, users can now assign tasks to individuals within a Contact Group. You can create Contact Groups for teams (denials, billing, specific offices, payments, etc.) and assign tasks to those groups to ensure work is completed. All users in the group will see the tasks assigned to the group, and once completed, the system will track which user completed the task via the User Productivity by Tasks Completed Report, allowing you to monitor user productivity. For more information creating Shared contact groups, visit our Create a Shared Contact Group Help Article. For info on assigning tasks to a contact group, visit our Assign a Task to a Contact Group Help Article.
New Prior Authorization Requirements & Billing Alerts Update
In this release, we have added a couple of updates to the billing alerts for procedure codes. First, we introduced a new option within the Procedure Codes setup window to set a Prior Authorization Requirement as a default on the code. You can set the Prior Authorization Requirement on a code for all payers or a list of specific payers. When there is a pre-authorization requirement and no authorization number is set on a claim, you will now receive a warning during the claim review. For more information on setting up a prior authorization requirement, visit our Add CPT/HCPCS Codes Help Article.
We also updated the placement of billing alert warnings within the application. Billing alerts will now be displayed not only in the claim section, but also in the claim control area when running the claim review process. This change is intended to help our interface customers more easily access these billing alerts, as they are now integrated into the claim review workflow.
New Appointment Type Default Codes
We previously added claim defaults for POS and TOS within the Appointment Types configuration. In this release, we introduced Appointment Type Default Codes, allowing users to set default procedure codes on appointment types. When creating claims from the appointment scheduler, these default codes will be used. New estimates created from the appointment scheduler will also use default procedures from the Appointment Type, making estimates faster and easier than ever.
Please note that these default codes apply only to claims created from an appointment. Patient Default Procedure Codes won't be used if the Appointment Type has a default procedure, though patient default diagnosis codes will still be used. Claims created from the claim section will not use these Appointment Type default codes, only Patient Defaults if available. Visit our Add New Appointment Type Help Article for more info on adding default codes to an Appointment Type. 
Enhancements
New Report Fields
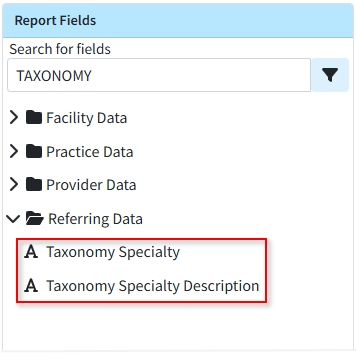
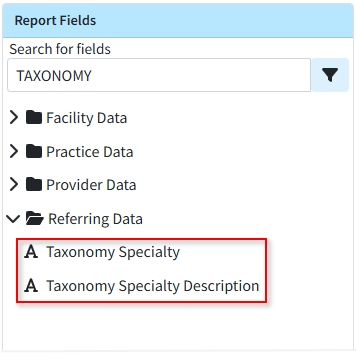
Previously, users could add fields related to the taxonomy specialty and the taxonomy specialty description for Providers and Practice, but not for Referring Providers. In this release, we added fields to report on taxonomy codes (specialties) and its description for Referring Providers.- Referring Data → Taxonomy Specialty
- Referring Data → Taxonomy Specialty Description
View Prior Claim Status Checks
We have long supported viewing prior claim status checks from the Claim section, but this ability was not available for claim follow-ups. In this release, we added this capability to the Claim Follow-Up Management section.
Web API Updates
In this release, we made a few enhancements to our WebAPI. On professional claims, we support the "Charge To Date" to represent charges over a period of time. This "to date of service" can be sent in the FT1.5 segment. However, on institutional claims, there is no location on the claim form for the "To Date of Service" for any particular charge, so we do not support it. Since some payers require sending one charge with multiple units to cover multiple days, and individual charges are the only way to send dates, and institutional claims don’t support the "To Date of Service," it becomes difficult to set a "Statement Covers To" date that extends beyond the last charge’s date of service. In this release, we updated our WebAPI to internally store a "To Date" of service and use it to determine the claim's statement covers "To" and "From" dates when a single charge covers multiple days.
We also added the ability to add payments via the WebAPI. Previously, when we received payments from the WebAPI, they were applied as a credit, and users had to access the application to apply the payment. In this release, we updated the WebAPI to allow users to apply a patient payment directly to specific claims instead of as a credit. Users can now use the Activity or Charge History APIs to get charge details and use that information to choose where to apply new payments (only new payments, not existing credits).
Resolutions
ERA Secondary OA-23 Adjustments Update
The process of applying a secondary adjustment on an ERA has been updated to no longer allow the OA-23 adjustment. This adjustment, related to prior payers' payments and adjustments, should never be applied as it can incorrectly affect the balance and cause an incorrect account credit.
Update from Release 15.9 (Net Amount available in the Activity Report)
We recently added a new user-level setting to the Patient Settings to display the Net Amount (based on the allowed or contracted amount) in the Patient Activity section. When set to "Yes," the Net Amount and Net Balance would be shown in the Claim listing in the Patient Activity. In this release, we removed this setting due to an issue found with the feature. We will correct this and re-release it in the June-July timeframe.