Follow the steps below to track your claims.
-
Select Claim > Claim Tracker.
-
Enter your Search Criteria or Load a Search Filter.
-
Use the Date Submitted option to filter the search by the date the claim was sent to the clearinghouse or the date it was printed from CMD.
-
Use the Date of Service (DOS) option to filter the search by date the services were rendered.
-
Use the Status Date option to filter claims based on the date status message was received from the clearinghouse or the payer.
-
Use the Submission Type drop-down menu to filter the search by electronic, paper, or user print.
-
Use the Processing Mode drop-down menu to filter the search by processing mode.
-
Use the Tracking Status Type drop-down menu to filter the search by the current tracking status of the claim (e.g., Sent, Accepted, Rejected- Not Fixed/Fixed, Warnings, No Errors, Unprocessed).
-
Use the Tracking Status Source drop-down menu to filter the search by where the status message was sent from. (e.g., CollaborateMD (Printing the claim, or sending it to the clearinghouse), Clearinghouse, Payer Rejections, EOB Denials.).
-
Use the Claim Status drop-down menu to filter the search by the claim’s current status (e.g., Waiting for Review, On Hold, At Insurance, Waiting to …).
-
Use the Claim Type drop-down menu to filter the search by Professional or Institutional Claims.
-
Use the Tracking Status (Contains) field to filter the search by keywords in the status message sent back by the payer.
 You are able to search for claims based on a portion of the rejection message, for example, “Invalid Zip Code...”
You are able to search for claims based on a portion of the rejection message, for example, “Invalid Zip Code...” -
Populate the TCN (Transaction Control Number) field to filter the search to show specific claims based on the TCN number entered.
-
Populate the Claim field to filter the search to show specific claims based on the claim number entered.
-
Use the Patient field to search for all claims associated with the selected patient.
-
Use the CPID field to search for claims submitted to a specific CPID.
-
Use the applicable drop-down menus to filter your search by specific Payers, Payer Type, Billing Providers, Rendering Providers, and/or Facilities.
-
Place a check in the Include claim history box to include any other claim submissions for claims returned in the search results.
-
-
Click the Search button.
-
Optional: Click on the
 icon to edit your search criteria.
icon to edit your search criteria. Sort your search results. Visit our Reorder Table Columns Help Article for detailed steps on how to hide, rearrange or add header columns.
Sort your search results. Visit our Reorder Table Columns Help Article for detailed steps on how to hide, rearrange or add header columns. -
Optional: Use the Group By drop-down menu to group your results by date submitted, payer, patient or provider.
-
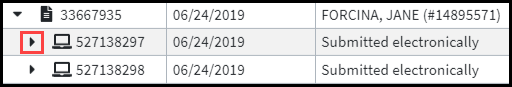
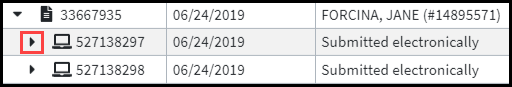
Place a check in the Expand All box click on the arrow next to the Claim to see more claim details.
-
Optional: Click the triangle node next to each claim to expand individually.
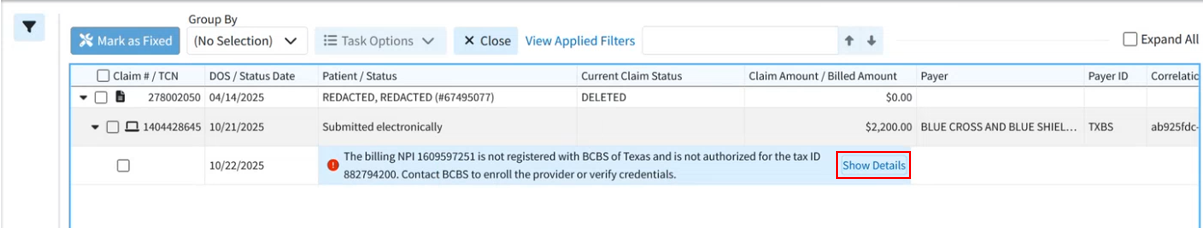
 Hovering over a specific status line within the status column after a claim is expanded will allow you to see the complete status message.
Hovering over a specific status line within the status column after a claim is expanded will allow you to see the complete status message.  If an intelligent claim rejection message is available, the confusing payer message is hidden by default and replaced with an AI-produced message that is easier for users to read, understand, and is better formatted. Users can click "Show Details" to view the full list details of payer messages, if needed. Visit our What Are Intelligent Claim Rejections Article for more information.
If an intelligent claim rejection message is available, the confusing payer message is hidden by default and replaced with an AI-produced message that is easier for users to read, understand, and is better formatted. Users can click "Show Details" to view the full list details of payer messages, if needed. Visit our What Are Intelligent Claim Rejections Article for more information.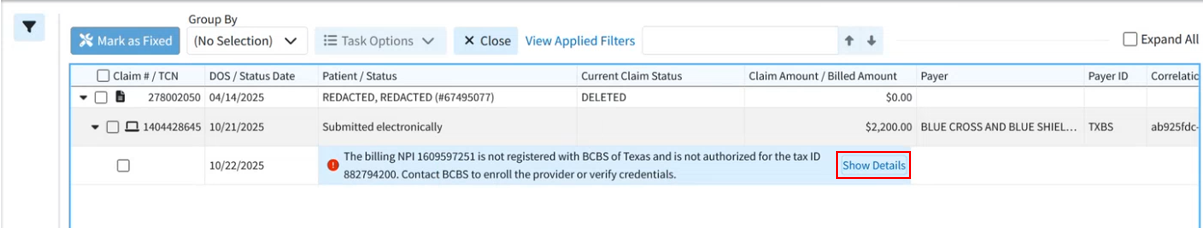
-
You are able to interact with the search results by right-clicking on a row.
-
Copy: Copies the claim information to your clipboard.
-
Open Patient: Opens the patient associated to the claim.
-
Open Claim: Opens the claim in the Claim Section.
-
Create Task: Creates a task related to the claim.
-
View Reports: View any Clearinghouse Report associated with this claim submission.
-
Mark as Fixed: Marks an error message as "fixed" for tracking and organizational purposes.
-
Find Payer Batch Reports: View any payer batch / Clearinghouse reports associated with this claim submission.
-
View Additional Clearinghouse Data: View any Clearinghouse data associated with this claim submission.
-
Print Proof of Timely Filing Letter: Print a basic proof of timely filing letter directly from Claim Tracker.
-
Print Appeal Letter: Print a basic appeals letter directly from Claim Tracker.
-
-
Click Close to exit the results.
 You are able to search for claims based on a portion of the rejection message, for example, “Invalid Zip Code...”
You are able to search for claims based on a portion of the rejection message, for example, “Invalid Zip Code...”  Sort your search results. Visit our
Sort your search results. Visit our