Claim Status provides the capability for users to submit status requests and receive responses in real-time regarding their claims. The claim status response provides information about your claim within the payer’s adjudication process, including how much is being paid on the claim once approved. Users can retrieve this information within the CollaborateMD application without having to contact the payer. There are no additional fees for this service.
Claim status can be verified for any claim that meets the following criteria:
-
The payer supports electronic Real-Time Claim Status (RTCS).
-
The claim was submitted electronically to the payer.
-
The claim status must be set to “Claim At Insurance.”
 Depending on the payer, an agreement may need to be filled out prior to checking claim status. Please refer to our Payer Agreements Help Article for more information.
Depending on the payer, an agreement may need to be filled out prior to checking claim status. Please refer to our Payer Agreements Help Article for more information.
Follow the steps below to check a new or existing claim status.
-
Select Claim > Claim.
-
Use the Search field to search for your claim.
 Place a check in the “Show exact matches only” box to search for exact matches or “Show unpaid claims only” to show claims that may need follow-up.
Place a check in the “Show exact matches only” box to search for exact matches or “Show unpaid claims only” to show claims that may need follow-up.
-
Open the claim.
-
Click the Claim Status button.
-
Select Claim Status Check to perform a new request for the status of the claim.
-
Select Last Checked On (Date) to view the last existing request for the status of the claim.
-
View All Past Claim Status Reports to view all previous requests for the status of the claim.
-
-
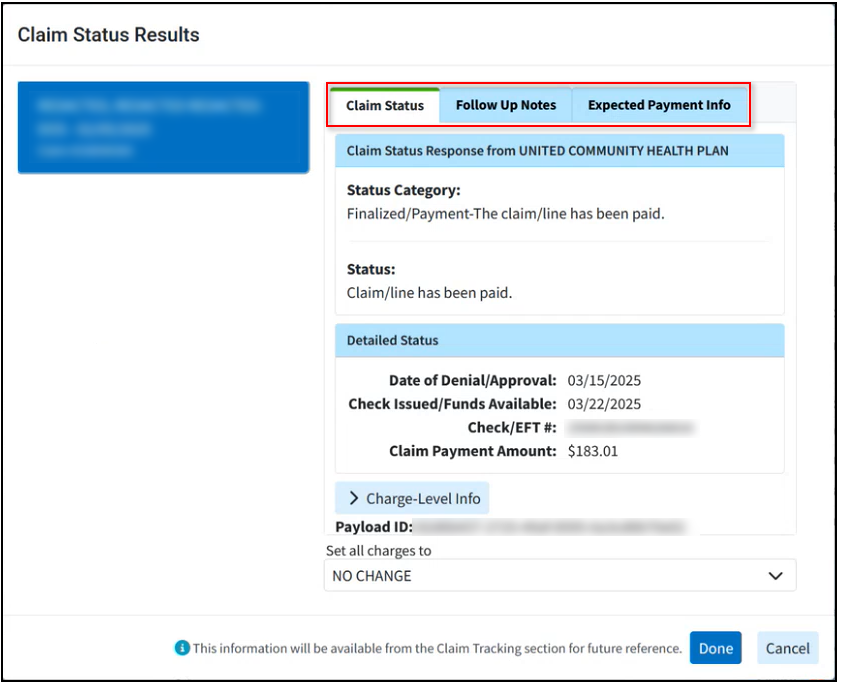
The Claim Status Results window has the following 3 tabs:
-
Claim Status: Provides the claim status response from the payer along with a detailed status, payments, and an option to update the charge status from the results screen.
-
Follow Up Notes: Allows the user to enter any follow up notes pertaining to the claim.
-
Expected Payment Info: Provides any expected payment information from the status result (paid amount, check date, and check number).
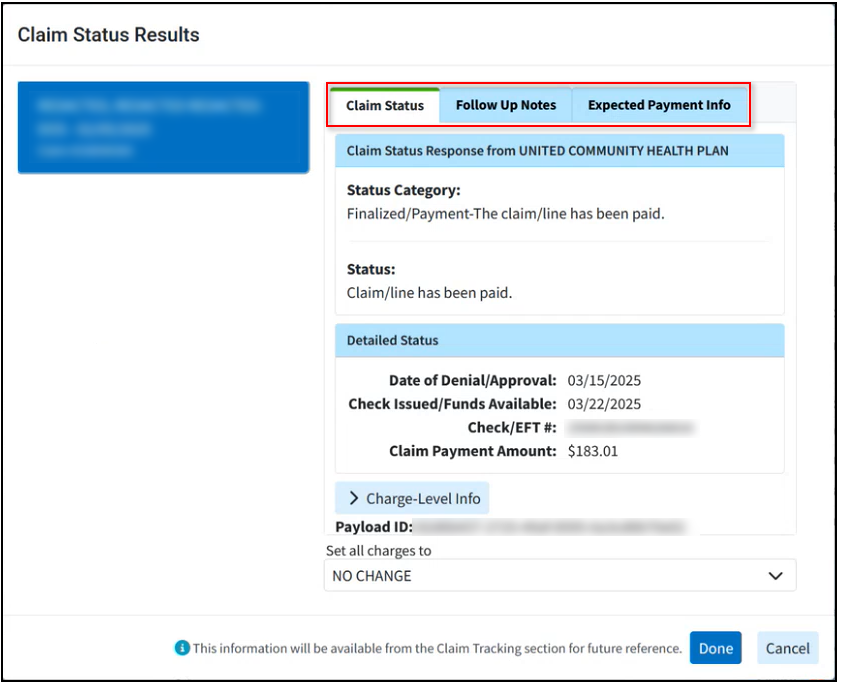
 Data from the follow up notes and expected payment info within the claim status results window will be available in the Follow Up Management section.
Data from the follow up notes and expected payment info within the claim status results window will be available in the Follow Up Management section.
-
-
Click Done.
-
Click Close.
 Place a check in the “Show exact matches only” box to search for exact matches or “Show unpaid claims only” to show claims that may need follow-up.
Place a check in the “Show exact matches only” box to search for exact matches or “Show unpaid claims only” to show claims that may need follow-up.