Highlights
New features
New Claim Workflow Enhancements: Combining Claims
We added a new feature within Claim Control section that allows users to find and combine claims (as long as the claims are for the same patient/payer/provider). CollaborateMD's new Combine Claims feature allows users to merge two or more separate claims into one, consolidating all charges and removing the duplicate claims automatically. This is useful for customers who need to combine encounters into a single claim due to the EHR separating the encounter into multiple claims, payer bundling requirements, or any other reason. Simply select your claims and click the Combine Claims button to start the process. 
You will be presented with a list of charges that will be combined into the new claim where you can reorder the charges before combining them into a new claim. 
Once combined, you can save the new claim, and only the new combined claim will exist, while the individual ones will be deleted. For more information on combining claims, visit our Combine Claims Help Article.
New Claim Workflow Enhancements: New Institutional Defaults
In this release, we have added updates to the patient and payer claim defaults for institutional claims. First, we separated the Patient Claim defaults into Professional and Institutional categories. The availability of Professional or Institutional claim default options depends on whether the default provider for the patient sends professional claims, institutional claims, or both. The claim default options for Professional Claims include ICD and CPT Codes. For Institutional Claims, the options are Principal Diagnosis, POA, Other Diagnosis, CPT Codes, and Value Codes to provide more flexibility when setting your defaults. For more information on setting up institutional patient claim defaults, visit our Patient Claim Defaults Help Article. We also added 2 payer billing options for claims. Within the General Billing Options tab, we introduced a new option to select a Default Value Code to be included on institutional claims for this payer. Additionally, under the Provider Billing Options, we added an option to select a Default Referring Provider for every claim under this provider. Visit our General Billing Options and Provider Billing Options Help Articles for more information.
We also added 2 payer billing options for claims. Within the General Billing Options tab, we introduced a new option to select a Default Value Code to be included on institutional claims for this payer. Additionally, under the Provider Billing Options, we added an option to select a Default Referring Provider for every claim under this provider. Visit our General Billing Options and Provider Billing Options Help Articles for more information.
New Task Automation for AutoPay
We added a new Task Automation feature allowing customers to configure their practice to automatically create a new task for any payment failures during the daily AutoPay process. This task will be linked to the patient and assigned to a pre-selected user or group. Customers that use the AutoPay feature can now set up the "Create a task when a patient's AutoPay payment fails" task automation from the practices right-hand side panel. Visit our Task Automations Help Article for more info on setting up this automation. 
Custom Claim Scrubbing Edits & Claim Scrubbing Specialty
In this release, we added two significant enhancements to our Claim Scrubbing. First, we introduced an option within the Claim Scrubbing configuration screen that allows customers to set up (or change) their specialty to receive more tailored edits for their specific claims. Visit our Manage Claim Scrubbing Help Article for more information on setting your Specialty. Secondly, we introduced a new Claim Scrubbing Custom Edits & Analytics service that provides customers access to the ClaimStaker® application, allowing them to review existing claim scrubbing edits, create new ones, and review detailed analytics. This is a paid service that can be requested from Services > Other Services and includes one initial training session on how to use ClaimStaker® to create custom edits and review analytics.
Secondly, we introduced a new Claim Scrubbing Custom Edits & Analytics service that provides customers access to the ClaimStaker® application, allowing them to review existing claim scrubbing edits, create new ones, and review detailed analytics. This is a paid service that can be requested from Services > Other Services and includes one initial training session on how to use ClaimStaker® to create custom edits and review analytics. 
For more information on requesting this service, visit our Request Claim Scrubbing Custom Edits & Analytics Help Article.
Enhancements
New Claim Workflow Enhancements: New Situational Modifier Options
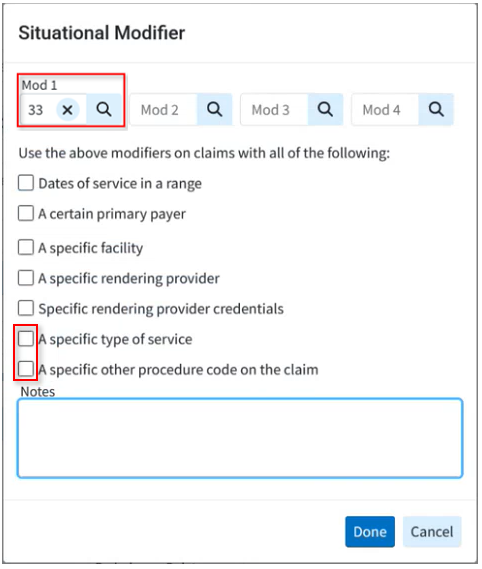
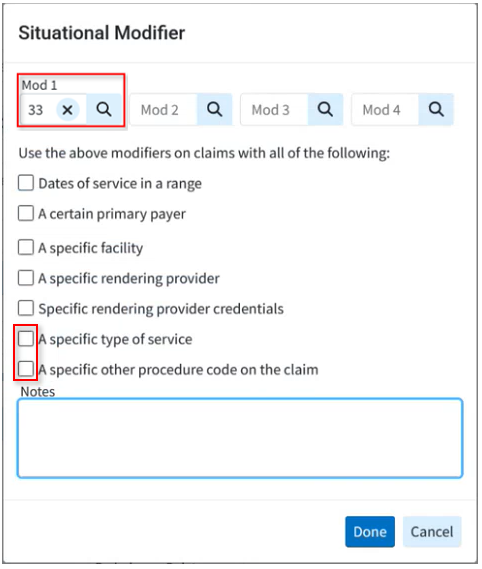
In this release, we have added a couple of updates to the situational modifiers for procedure codes. First, we introduced two new options within the Procedure Codes to set Situational Modifiers.
- A new option to create a situational modifier based on "A specific type of service" to set a specific TOS code that the modifier should apply to.
A new option to create a situational modifier based on "A specific other procedure code on the claim" to select a procedure code that will trigger the modifier only when this other procedure is present on a claim.
We also updated the Dates of Service, Primary Payer, Facility, Rendering Provider, Rendering Provider Credentials, and TOS situational modifier options to be multi-select, making it easier for practices with a large number of records to manage these modifiers. For more information on adding these modifiers, visit our Add Situational Modifiers Help Article.
New Claim Workflow Enhancements: Claim Status Updates
We updated our Real-Time Claim Status results window to allow users to update the claim charge status directly from the results screen. Users can now also enter any follow-up notes pertaining to the claim, as well as any expected payment information from the status result (paid amount, check date, and check number). This update will automatically override any existing data in Expected Payment Info with information from the Claim Status if the payer made a payment. For more information visit our Claim Status Help Article.