Resolutions
Claim Scrubbing: Copy Configuration Issue Corrected
We previously introduced an option within the Claim Scrubbing configuration screen that allows customers to set up or change their specialty to receive more tailored edits for their specific claims. Billing services, in particular, need to be able to use the Copy Configuration option to easily set up all of their customers' claim scrubbing configurations. However, when Copy Configuration was recently used, it was not copying correctly, and we were not setting up Aptarro submitters for any of the customers that had it enabled. In this release, we updated the claim scrubbing configuration window. When a specific specialty is selected, and then the "Copy Configuration" button is clicked, the system will display the selected specialty for each customer in the list. (The normal logic will be used to select a default specialty if one has not been chosen.) Additionally, when a configuration is copied, the system will register all necessary submitters with Aptarro. 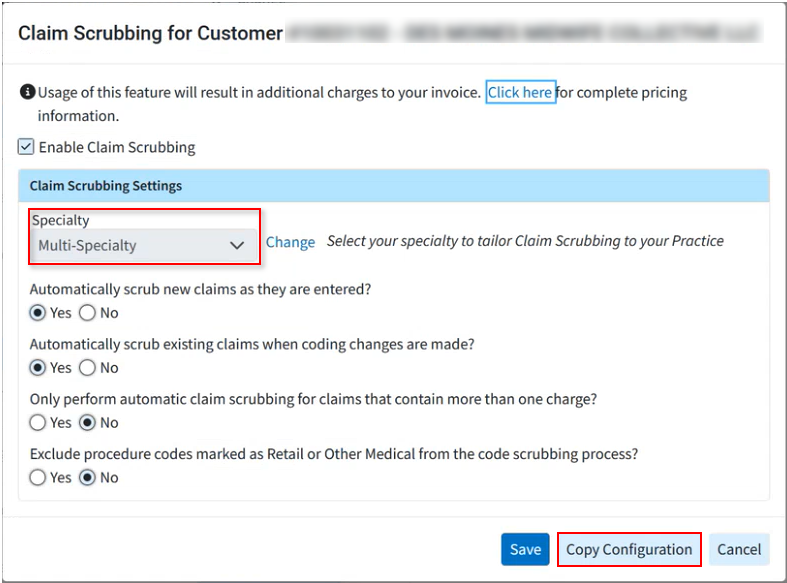
Interface Tracker: Not all Columns Visible at Minimum Resolution
We corrected an issue within Interface Tracker causing some columns not to be visible when the monitor was at minimum resolution. With this update, users can now horizontally scroll to see all columns on all supported browsers/screen resolutions.
As part of this release, we are continuing our ongoing work to assess, monitor, and address any security vulnerabilities.
Highlights
New features
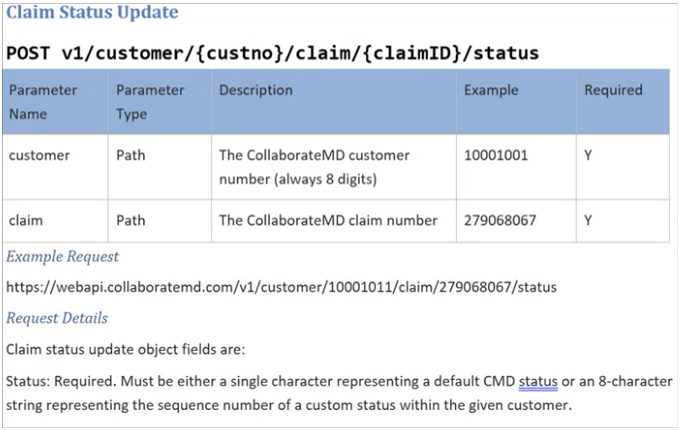
New WebAPI Endpoint to Allow Setting a Claim To a Specific Status
This release introduces a new endpoint for all WebAPI customers who create claims. This endpoint allows customers who integrate with our API and work outside our system to set claim statuses. They can set claims to any custom status and most standard statuses. Please note that Paid, Send to Insurance, User Print, and Delete statuses are not supported. This new claim status option is available to all WebAPI customers, allowing integration customers to send claims to specific status buckets for processing.
Enhancements
New Payment Plan Auto Pay Report Fields
In this release, we added new report fields under "Payment Plan Data" to allow users to report on the status of payment plans that are on Auto Pay. We first added a new "AutoPay Status" field that will show one of the following statuses (also usable in a Filter):
Not Set Up: If AutoPay has never been set up for this payment plan
Active: If AutoPay is currently set up for this payment plan
Disabled: If AutoPay had been set up but was disabled by a specific user
Failed: If AutoPay failed for this payment plan
We also added report fields for:
AutoPay Enable User: Will show “Patient” if the patient did it from the Portal
AutoPay Enable Date: Date/Time it was enabled
AutoPay Disable User: Will show “CollaborateMD” (rather than “AUTO_DEBIT”) if the system disabled it
AutoPay Disable Date: Date: Date/Time it was disabled
For more information visit our Payment Plan Data Help Article.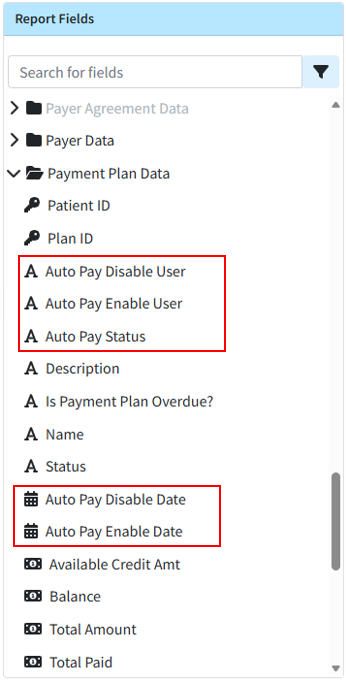
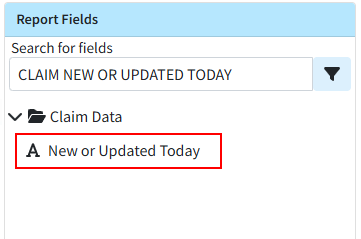
New Report Field for New or Changed Today Claims
This release also brings a new report field within Claim Data, "Claim New or Changed Today," that efficiently reports on claims and charges that were added or changed today. This allows you to get data specifically on claims that have been added or changed the current day, allowing users to get the claim information that has changed since the last snapshot without having to wait for the next days snapshot.
Visit our Claim Data Help Article for more information.
Claim Frequency Reset Enhancement
Previously, when resubmitting claims to the primary payer, staff manually reset the claim frequency to 1 after posting the ERA/EOB and before sending to the secondary payer. In this release, we updated the system so that when a professional claim's status changes to "Send to Insurance via Clearinghouse" or "User Print & Mail" through the ERA or EOB screens, the claim frequency automatically resets from 7 to 1 before sending the claim to the next payer.
Statement Vendor Change Configuration Warning
To facilitate the completion of our Statement Vendor migration to DataMedia (DMA), we added a non-dismissible message to the login screen. This message will appear for users with permission to edit statement templates on accounts where Statement Automation is enabled but not yet configured with the new statement vendor for any statement type. The warning will inform users that they must configure and verify the new statement template in their account to continue sending statements. It will also include a "Verify Templates" button, which will direct users to the configuration screen to complete the setup process. 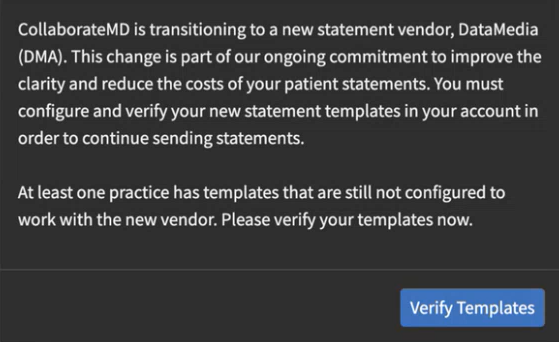
As part of this release, we are continuing our ongoing work to assess, monitor, and address any security vulnerabilities.
Highlights
New features
New "Claims Not Acknowledged by the Clearinghouse" Timeline Item
This release introduces a new timeline item that checks for electronic claim submissions with an "Unprocessed" status, submitted between 2 and 30 days prior. This new timeline item alerts users by identifying any claims not received by the clearinghouse. This enables users to quickly identify these claims and contact support to work with the clearinghouse to determine why they were not received. This new "Claims Not Acknowledged by the Clearinghouse" timeline item will be displayed by default under the Billing role. It will also link to a "Claims Not Acknowledged by the Clearinghouse" report when clicked.
For more information on enabling this timeline item, visit our Customize Your Timeline Help Article.

Enhancements
New Option to Calculate With Fixed Values on Reports
Previously, calculated columns on reports allowed users to select two numeric or date columns for calculations. However, certain reporting use cases require calculations based on a fixed number rather than another column. For instance, for some services, the number of units is a fraction of the time spent (e.g., each unit represents 15 minutes), so it can be useful to report on this.
In this release, we added a new option to both Column 1 and Column 2 for any calculated column with a "Number" calculation type. When "Fixed Value" is selected, a new option appears to enter the fixed value and choose the calculation method (Plus, Minus, Multiplied By, Divided, By). This field accepts a minimum value of -99,999,999, a maximum value of 99,999,999, and up to 10 decimal places. 
For more information visit our Add Calculated Columns Help Article.
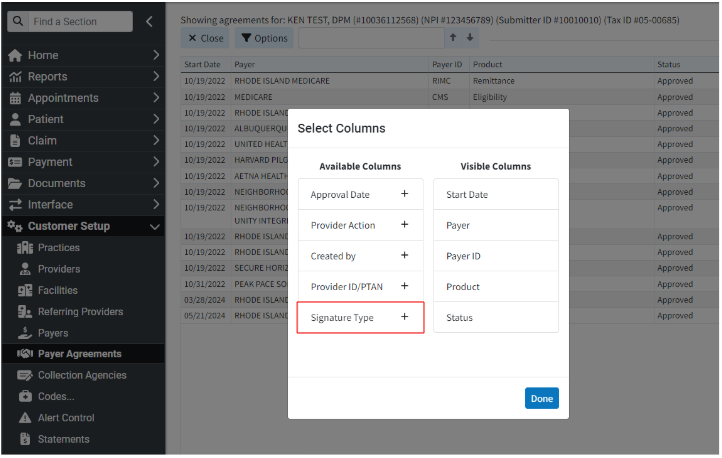
New Follow Up Management Payment Columns
In this release, we added two optional columns to the follow-up management table, allowing users to view the total amount of applied payments. The new "Insurance Payment" and "Patient Payment" columns will be hidden by default and can be added using the "Select Columns" option or by right-clicking and selecting "Select Columns." 
Payment Automations: Customize Denial Status
In some cases, by the time users receive a denial, they have already addressed and resolved the issue. Therefore, it is not always helpful for the claims to automatically be marked as "Denied at Insurance." They may prefer to set their own custom status for these claims, for example, all issues with prior authorization could go to a specific status for review.
In this release, when the Processing Mode for a payment automation is set to either "Process as a Partial Denial" or "Process as a Total Denial," users will be able to select their own claim status, and when the automation runs for this Processing Mode, it will apply the selected status to the charges. 
Please note that all existing automations with a "denied" status will be updated to set the claim status to "Denied at Remittance Payer,” but the users are able to update the status as needed. For more information visit our Add a Payment Automation Help Article.
Incremental Snapshots Now Include Claim Status
One of the biggest tables for data snapshots is the Claim Status. In this release, we updated how we store the date when a claim status entry is marked as fixed or marked as not fixed to now support claim status on incremental snapshots. Incremental Data Snapshots minimize the time required for the snapshot process by including only changed items, rather than capturing a complete snapshot of the entire database daily. The Incremental Snapshot option exports smaller (incremental) files containing only data that has changed for the Patient, Claim, Charge, Credit, and Activity tables. All other datasets will receive the full data, ensuring your snapshot is prioritized and available sooner than full snapshots. So save time and money by switching to Incremental Snapshots today!
For more information on setting up your Incremental Snapshots, visit our Manage Recurring Data Snapshots Help Article.
Resolutions
A/R Report Performance Improvements
We added an internal enhancement that allows AR reports (or any reports that look at charges with a balance) to run faster. This addresses performance issues with a long-running AR reports, enabling it to run within an acceptable timeframe.
Payment Automations: "All" Group Codes Now Includes Scenarios Where Group Code Isn't Listed
We corrected a Payment Automations issue where, if an automation was configured for all group codes (by selecting the "All" checkbox), the automation did not match when the code lacked a group code (e.g., a 197 remittance code without a group code like "CO"). This has been resolved, and the automation will now match even if no group code is present.
Therefore, if the automation is configured for all group codes, it will now match regardless of whether a group code exists. 
As part of this release, we are continuing our ongoing work to assess, monitor, and address any security vulnerabilities.
Highlights
| New Features | Enhancements |
|---|---|
| New Intelligent Claim Rejections New Supervising Provider Default |
Incremental Data Snapshot Enhancements New Claim Type Column in Claim Control |
New features
New Intelligent Claim Rejections
We previously released our "Intelligent Claim Rejections" feature, which we are systematically rolling out to more customers behind the scenes. We will complete a full roll out to all customers in the coming days. In this release, we are updating how rejection messages are shown in Claim Tracker to make them easier for customers to understand. If an intelligent claim rejection message is available, the confusing payer message will now be hidden by default and replaced with an AI-produced message that is easier for users to read, understand, and is better formatted. We also added extra space to the intelligent message so it is not confined to one line. Users can click "Show Details" to view the full list details of payer messages, if needed. Visit our Track a Claim Help Articles for more information.
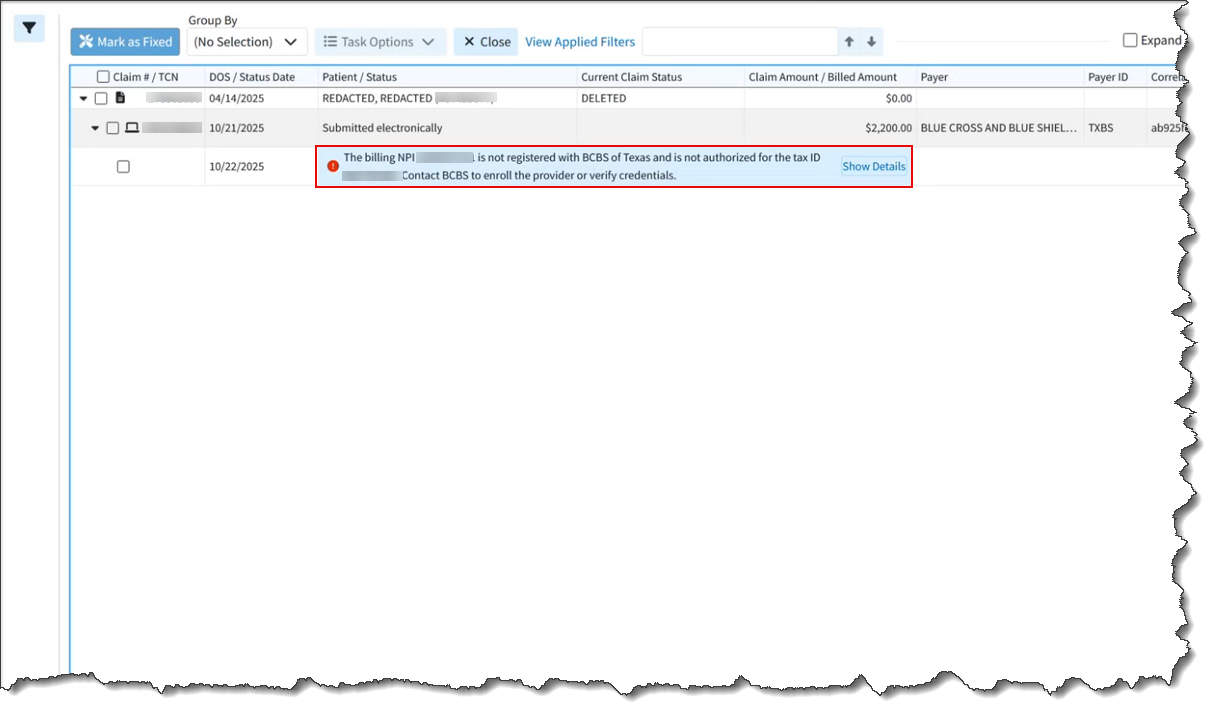
 If you do not yet see intelligent claim rejections in Claim Tracker, we will be systematically rolling out this feature to all customers in the coming days.
If you do not yet see intelligent claim rejections in Claim Tracker, we will be systematically rolling out this feature to all customers in the coming days.
New Supervising Provider Default
This release introduces a new patient claim default for customers who are required to bill with a supervising or operating provider. This automation enables users to set a default supervising provider on professional claims or an operating provider on institutional claims. Once configured, the system will automatically add the supervising/operating provider for claims entered manually in the application and for interface claims when a supervising/operating provider isn't sent over. For more information on enabling this default automation, visit our Configure Patient Claim Defaults Help Article.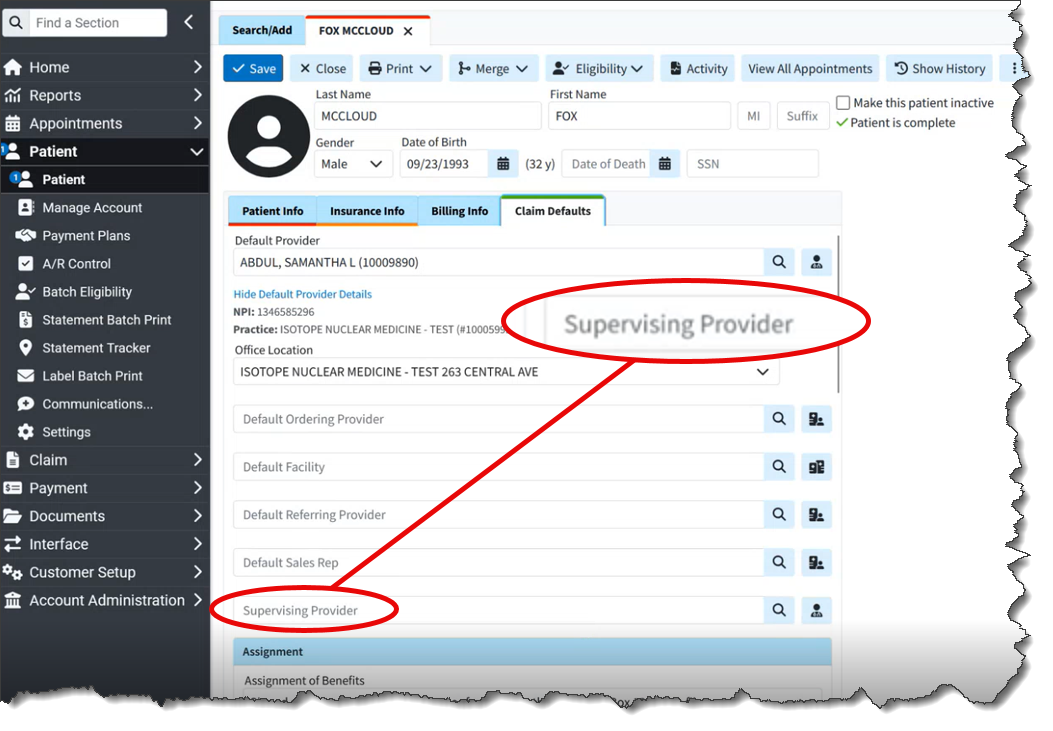
Enhancements
Incremental Data Snapshot Enhancements
This release introduces several enhancements to our Incremental Snapshots. Previously, our Incremental Recurring Data Snapshot feature produced a snapshot of all changes since the last recurring snapshot, typically one day. However, if users failed to download their incremental snapshot (e.g., due to system downtime), they would have to revert to a full snapshot.
In this release, when Incremental Snapshot is selected, we added the ability to specify the minimum number of days to include in the incremental snapshot. The default will be one day, but the system will allow selection between one and seven days. This will include data that is new or has changed since the last recurring snapshot or within the selected number of days, whichever period is longer. 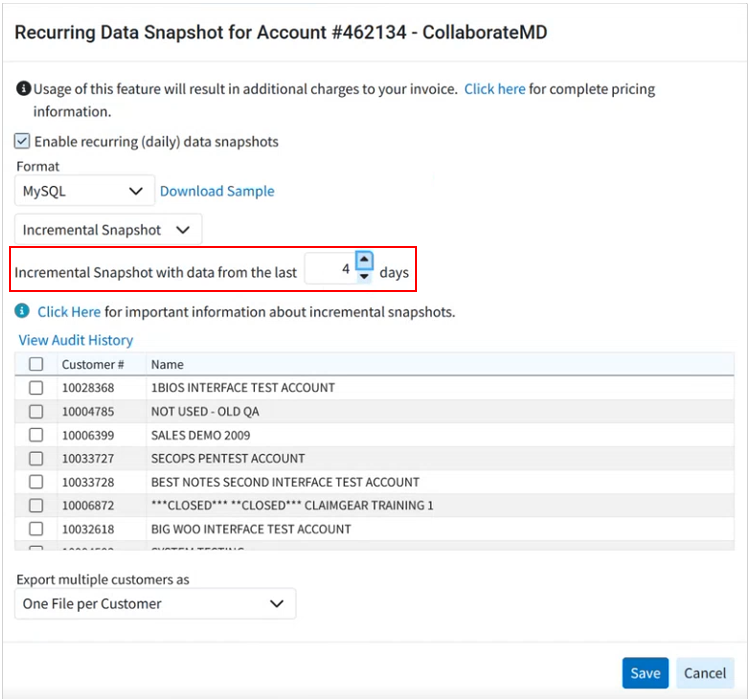
Full Data Snapshots are typically delivered later in the day due to their large file size, which requires more time for download and integration into databases. In this release, a new warning message has been added for customers who select Full Snapshot as their recurring data snapshot option. This message informs them of the delivery implications and recommends choosing Incremental Snapshots to reduce file size and enable faster delivery. Consequently, users with incremental snapshots will receive their snapshots earlier in the day, as they will obtain a smaller file containing only new or changed data. 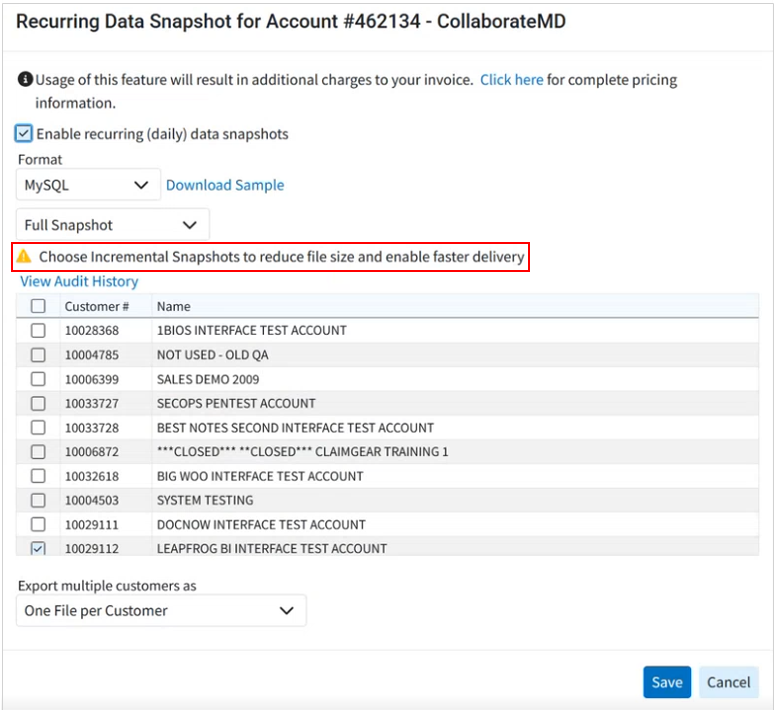
Previously, when customers set up recurring data snapshots, the system defaulted to a Full Snapshot, requiring them to manually select incremental snapshots from the available options. In this release, Incremental Snapshots will become the default option for recurring data snapshots. This change is implemented because most customers primarily require incremental snapshots, which capture only changed items and offer a faster, more efficient solution. For more information visit our Manage Recurring Data Snapshots Help Article.
New Claim Type Column in Claim Control
A new column for the "Claim Type" has been added to the Claim Control table. This column will be hidden by default and can be accessed via the "Select Columns" option or the right-click "Select Columns" option. When added, this column will display the claim type as a visual identifier for customers who submit both professional and institutional claims. 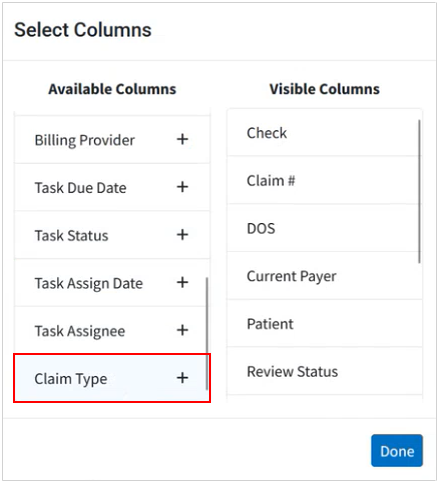
Resolutions
Added New Adjustment Action and Improved Overall Denial Processing Not Properly Reflected in Payment Automations
We resolved an issue that caused payment automation denials to not reflect properly. When processing a total or partial denial, several codes with a "Denied" action incorrectly displayed the adjustment action as "Do not Apply," even though the adjustment action should always be applied as an unpaid amount for partial or total denials. We also added a new adjustment action, "Apply as an unpaid amount but exclude from allowed amount," to all automations. The existing action, "Apply as an unpaid amount (due patient/next insurance)," was updated to "Apply as an unpaid amount and include in the allowed amount (due patient/next insurance)." These updates ensure the Allowed Amount is set correctly and users can select a custom charge status when processing a denial. 
Highlights
| New Features | Enhancements |
|---|---|
| New Statement Vendor Change
|
ERA Secondary Claim Improvements
|
New features
New Statement Vendor Change
In this release, we will be transitioning to a new patient statement vendor, DataMedia (DMA), to enhance the customer experience and better serve your patients. This transition will occur behind a feature flag in groups or waves, and customers will be notified when they have been switched to the new vendor. Once the feature flag is activated, your new statement template will be auto-filled based on your previous settings, requiring minimal effort for confirmation.
Please note that, at this time, the vendor change only applies to automated statements (statements, payment plans, and FDNs), not to enhanced user print statements.
The new statement templates will eliminate additional pages, making statements more concise and cost-effective. The new template also features a clearer statement activity listing, distinguishing charges, payments, and adjustments, and the balance for each individual charge. This new template will also separate insurance payments and adjustments, providing a clearer, more detailed, and organized statement at no additional cost, as the pricing for statement automation will remain the same.
 Important - Customers with automated statements enabled before the statement vendor change must complete the following after being transitioned to the new vendor:
Important - Customers with automated statements enabled before the statement vendor change must complete the following after being transitioned to the new vendor:
- Configure your new statement templates (must be done for each practice).
- When opening the new templates, all required fields will be pre-populated from your previous template. However, the template still need to be reviewed and saved.
- Please be aware that statements will not be sent until the templates are reviewed and saved.
Visit our Configuring Statement Automations Demo for an interactive, step-by-step demonstration on configuring your statement template, or refer to our Configure Statement Automation Templates Help Articles for more information.

Enhancements
ERA Secondary Claim Improvements
Previously, charges paid by the primary payer were not automatically forwarded to the secondary payer on ERAs/EOBs. This release improves the handling of charge statuses in ERA/EOB claims processing, ensuring all applicable charges are correctly sent to the subsequent insurance payer. With this update, if at least one charge in an ERA/EOB is to be sent to the next payer, then all charges will be forwarded to the next payer, and their status will not be set to PAID. We also made an update when reviewing big ERAs to prevent any browser "Out Of Memory" errors.
Highlights
New features
New Payment Automations Feature
In this release, we added an exciting feature that allows users to build powerful custom automations to prevent manual work for ERAs. They can be configured to perform actions automatically based on the remittance codes received from the payer. These automations replace our existing "Remittance Actions" and significantly enhance the feature by expanding the criteria that payment automations can detect and improving the actions that automation rules can perform.
Our new Payment automations allow you to automatically mark payments as denials and move adjustments so they do not affect the balance. You can also create your own rules and criteria for moving adjustments, control how adjustments are applied, set specific status buckets where claims need to go, or even create and assign automatic tasks based on a remittance code.
Please note that this feature is available to all customers that use our ERA feature. Visit our Payment Automations Demo for an interactive, step-by-step demonstration on its use, or refer to our Payment Automations Help Articles for more information.

New Statement Automation Option to Send Based on Days Since Last Seen
For some institutional claim workflows, a patient may be admitted to the hospital for a period during which the provider sends multiple "interim" claims while the patient is still admitted. These claims may be paid and set to "Balance Due Patient" even before discharge. Many practices and hospitals prefer not to send statements until after a patient has been discharged.
In this release, we added a new option to Statement Automation to restrict patient statements until a specified number of days have passed since the patient's last visit. This setting, located under "Statement Options," allows users to set a hold on statements for 1 to 99 days based on the patient's last visit date. This new option is turned off by default and is included with our Statement Automation feature. For more info on enabling this feature visit our Statement Options Help Article. 
New Admitting Diagnosis Default
We previously added a new "Institutional" Default Codes tab within the patient's Claim Defaults section, allowing users to set default Principal Diagnosis, POA, Other Diagnosis, CPT Codes, or Value Codes to be added to any new institutional claim for the patient. We then added the admitting diagnosis default in release 15.18 but immediately reverted it to fix a bug. In this release, we re-launching the "Admitting Diagnosis" as a patient claim default for institutional claims. When the default admitting diagnosis is set and the user has enabled the claim setting to "automatically apply the patient's default diagnosis codes on new claims," the admitting diagnosis will automatically be set on new claims created for that patient. For more information on default codes, visit our Configure Patient Claim Defaults Help Article.

Enhancements
Remove All Option for Claim/Patient Not Found ERA Errors
When posting ERAs, particularly for new customers, the ERA may have a large number of “Claim Not Found” issues if the ERA has claims that were sent from different systems. Some of these ERAs are huge, meaning that it can take an hour just to mark all of these payments as removed.
In this release, we added a "Remove All" option next to the "Unresolved Errors" displayed at the top of the ERA screen. When unresolved errors of the type "the claim or patient for this payment was not found" are present, the system will display the "Remove All" button. Clicking this button will remove all such errors simultaneously instead of having to remove them one by one. Please note that this option will only be visible if two or more of these errors ( "the claim or patient for this payment was not found") exist. All other error types must be resolved individually. Visit our ERA Errors, Warnings, Informational Messages & Alerts Help Article for more information on errors and warnings.

Refund Reversals Removed from Statements
Whenever an insurance adjudicates a claim multiple times (e.g., paying, adjusting, and then issuing a refund/reversal), it creates a longer, confusing statement for patients. To enhance the patient experience and reduce clutter, we are removing all refunds/reversals from enhanced, automated, and electronic statements (payment portal). The system will now automatically detect reversed payments and adjustments. When this occurs, the original payment and adjustment, along with any associated information lines, will be excluded from the statement.
New Automatic TCN Prefix (For ERA Splits)
Previously, the TCN Prefix field in the Practice section was used by ePS when an ERA Split was necessary. This was not ideal because a Practice can be associated with multiple Providers (and therefore multiple submitters), which required significant extra work (e.g., creating multiple practices) and could lead to errors.
In this release, we added a new "TCN Prefix" field within the "Internal Use" area of the "Provider" section. This field will show the Practice TCN Prefix (if one exists), otherwise, a system-generated prefix will be created. We will automatically send this submitter-specific TCN prefix for submitters who lack a Practice-level TCN Prefix when an ERA split is required. This means that when entering an ERA split, ePS will look up that submitter in CMD and copy the TCN Prefix. The system-generated prefix will be consistent for all providers sharing the same Submitter ID. 
Display Follow Up Note Count on Claim Side-Tab Header
We added a "Follow-Up Note Count" indicator to the side-tab header within the claim's "Follow-Up Activity" side panel. This indicator mirrors the existing functionality on the top-level side-tab header for "Patient Notes," "Tasks," and "Alerts" when viewing a claim. 
Highlights
| New Features | Enhancements |
|---|---|
| New Onboarding Process for "In-App Credit Card Processing" (Beta Release) |
Charge Totals now Visible from the Payment Plans EIN The Defaulted Option when Adding a New Provider |
New features
New Onboarding Process for "In-App Credit Card Processing" (Beta Release)
Onboarding customers to our in-app payment processing feature was a time-consuming, multi-step process. It required close collaboration between our Strategic Customer Success team, the customer, and GPI to submit customer information to GPI, secure approval, and integrate credentials into CMD. This limited the speed and ease with which new customers could sign up or existing customers could add new merchant accounts.
This release introduces a new process enabling customers to complete and sign their entire application within CMD without additional intervention. This streamlined workflow allows users to sign up and immediately fill out the application directly from the Services section, with auto-filled data from their office information. A new multi-step dialog screen facilitates entering all required information and provides status updates for pending applications within the IPP Settings.
Please note that this is a BETA (limited) release and will soon be available to all customers. Visit our Manage In-App Credit Card Processing Help Article for more information.

Enhancements
Charge Totals now Visible from the Payment Plans
Previously, the total charge balance was not included when viewing a payment plan. Ideally, this information should be available to visually match the total charge balance with the payment plan balance, ensuring all charges have been added. In this release, we added a column to the main Payment Plan screen displaying the total charges and total balance of charges to help users visually confirm that all charges have been included in the payment plan. We also added these two values to the "Edit Payment Plan" screen.

EIN The Defaulted Option when Adding a New Provider
When creating a new Provider (either in the Provider section or in the New Account Wizard), the "Use which ID number?" field previously defaulted to the SSN. However, most billing is now done under the EIN. In this release, we have set this field to default to "Employer Identification# (EIN)" in both the Provider section and the New Account Setup Wizard, as it is more commonly used than SSN billing.

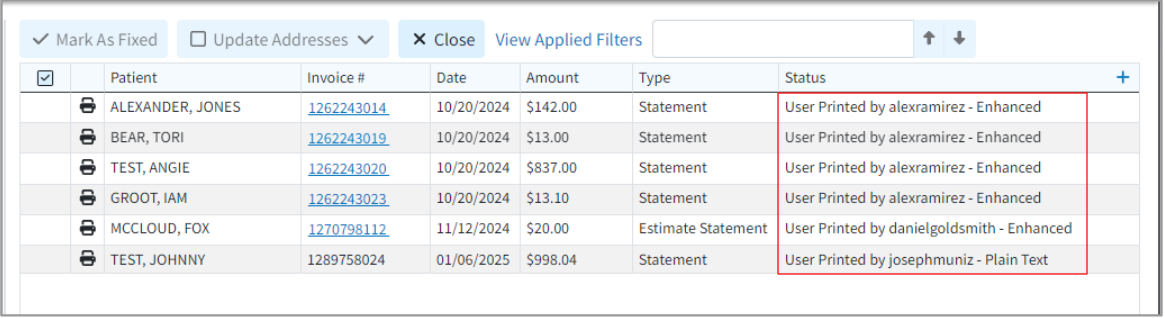
New Patient # Column within Statement Tracker
A new column for "Patient #" has been added to Statement Tracker. This column will be hidden by default and can be accessed via the "Select Columns" option or the right-click "Select Columns" option. When added, this column will display the patient account number.
Highlights
New features
New Task Management in A/R Control
We previously added the ability to add task reminders associated with specific records within more sections of the application (e.g., Claim Control, Claim Tracker, and Statement Tracker) to keep track of items that need to be completed. These tasks can have due dates, links, descriptions, statuses, and priorities, and can be assigned to yourself or to specific users/groups within your business. In this release, we added a new "Task Options" feature within the A/R Control section of the application. This feature allows users to create, manage, reassign, and delete tasks associated with a patient's A/R simply by checking them off. These tasks can also be linked (batched) to multiple patients simultaneously. Please be aware that these task management options are available in Plan 3 and above. Visit our A/R Control Task Options Help Article for more information.

Enhancements
New Admitting Diagnosis Default
We previously added a new "Institutional" Default Codes tab within the patient's Claim Defaults section, allowing users to set default Principal Diagnosis, POA, Other Diagnosis, CPT Codes, or Value Codes to be added to any new institutional claim for the patient. In this release, we added the "Admitting Diagnosis" as a patient claim default for institutional claims. When the default admitting diagnosis is set and the user has enabled the claim setting to "automatically apply the patient's default diagnosis codes on new claims," the admitting diagnosis will automatically be set on new claims created for that patient. For more information on default codes, visit our Configure Patient Claim Defaults Help Article.

Duplicate Remittance Codes Now Allowed if Group Code is Different
Previously, the system prevented adding duplicate adjustment codes on manual insurance payments. In this release, we updated the duplicate checking of remittance codes on insurance payments to account for differing group codes (e.g., OA-109 and PR-109). If a group code is present, the system will prevent a new code entry if that code already exists within the same group or without a group. However, entry is permitted if the group code is different. 
Custom Statuses Available as Report Filters
We added support to allow default filter selections and static filter selections on reports to work with custom statuses. This means that when selecting "Claim Status" as a filter on a report, you will be able to select from both standard and custom claim statuses as options for static or default filters.
Highlights
| New Features | Enhancements |
|---|---|
| New Statement Option for Continuing Visits New "Card on File" Indicator when Posting Payments ANSI (837) Import via WebAPI |
"Tracking" Tasks Enhancement |
New features
New Statement Option for Continuing Visits
CollaborateMD's Statement Automation has always allowed setting a maximum number of statements threshold, ensuring patients receive one only if their statement count is below this limit. However, this was not very effective for institutional inpatient, long-term care, or physical therapy settings, where numerous claims are billed in a short period of time. Consequently, if a patient failed to pay initial claims, they would not receive statements for subsequent ones. To accommodate these use cases, we added a new setting that will reset the "Number of Statements Sent" counter when a balance is newly set to "Due Patient." When set to "Yes," this new patient setting will reset the patient's "Statements Sent" counter to 0 when a claim is changed from another status to "Balance Due Patient" for the first time. For more information, visit our Configure Patient Settings for Customer Help Article.

New "Card on File" Indicator when Posting Payments
We added a new indicator to show if a patient has a credit card on file when using the In-App Payment Processing feature. If the "save payment information for next time" checkbox is selected, users will see the saved card(s) at the bottom of the payment screen. This is viewable when posting a payment from the Payment Post, Claim Payment tab, or Appointment Scheduler Payment tab.

ANSI (837) Import via WebAPI
We added the ability to import ANSI (837) files via new WebAPI endpoints, a feature previously exclusive to the Interface File Import. This enhancement also includes support for the "View Message Content" option within the interface tracker for ANSI 837 files from both API and File Import, enabling users to identify matching fields and better understand issues and errors.

For more information how to view the 837 message content, visit our Retrieve Interface Messages Help Article.
Enhancements
Tracking Tasks Enhancement
We recently added new task types for Statement Tracking and Claim Tracking. In this release, we updated the "Create Task" right-click option for consistency with task options in corresponding locations. These task types will now be used when creating tasks via the right-click option (this means that Claim Tracking now creates a claim tracking task & Statement Tracking now creates a statement task).
Appointment Text Improvements
Updated the appointment text messages so that when users click "Confirm" or "Cancel" it now requires an additional button press. This will prevent accidental confirmations or cancellations from text message previews on some smartphones.
Highlights
| New Features | Enhancements |
|---|---|
| Post Payments and Copays from Practice Fusion New Timeline Option for Due and Overdue Tasks New Dynamic Support PIN |
Enhancements to Claim Tasks |
New features
Post Payments and Copays from Practice Fusion
We added support for transmitting and posting payments and copayments applied in PracticeFusion to the claim in CMD after the claim has been created, based on information received from PF. Now, if "copay" is selected in PF, it is posted as a copay credit in CMD and can be applied automatically based on your copay settings. If "Payment on account" is selected, it will be posted as an account credit in CMD, reducing the manual work required to post these payments. A new Interface Setting has also been created that will allow these payments to transmit to CMD. This new "Allow interface to post Payments?" setting is enabled by default but can be disabled manually. For more information, visit our Manage PF Payments & Copays Help Article.

New Timeline Option for "Due and Overdue" Tasks
Two new Timeline items have been added to the Welcome Screen, that will provide all due and overdue tasks for the day. The new "Overdue Tasks" and "Tasks Due Today" options are automatically displayed for users with the Management role. Other users, or those with custom welcome screens, can manually select these options. When selected, the Task Search report will automatically apply the appropriate filters and pull up the report displaying all the due or overdue tasks for the day. For more information on adding these timeline options, visit our Customize Your Timeline Help Article.
New Dynamic Support PIN
We added a new auto-generated user-level dynamic PIN within the application in order to meet all HIPAA SRA requirements. This Dynamic Support PIN must be provided by users to validate their identity when contacting support via phone or live chat, and will automatically reset every 30 days or when verified by support. You can access your Support PIN two different ways:
1. Locate your Support PIN by going to "Help" in the User Bar and selecting "Show Support PIN."

2. Alternatively, you can access it by navigating to your User Profile and selecting "Show Support PIN.".
For more information visit our Show Support PIN Help Article.
Default Value Codes by Revenue Codes
A new Claim Defaults tab has been added to the Revenue Codes screen, enabling users to set a default Value Code for claims based on the revenue code. Once configured within a Revenue Code, the selected Value Codes are automatically added to claims utilizing that revenue code. This functionality applies to claims entered in CMD as well as interface claims. For more information on enabling this default, visit our Revenue Codes Claim Defaults Help Article. 
Default Diagnosis Codes by Procedure
We also added a new option to the Procedure Codes screen that allows users to set default diagnosis codes for claims based on the procedure code. The new Diagnosis Codes field within the Procedure Codes section allows users to enter diagnosis code(s), ensuring that when a procedure code is entered on a claim, the related diagnosis will populate automatically. For more information on enabling this default, visit our Add CPT/HCPCS Codes Help Article. 
Enhancements
Enhancement to Claim Tasks
We added the ability to filter tasks associated with claims via a new dropdown from the "Tasks" side-bar. There are 3 different claim tasks that are created in the application:
- Claim Tasks: Tasks created in the Claim section
- Follow Up Tasks: Tasks created in the Follow Up Management section
- Submission Tasks: Tasks created in the Claim Tracker section
This new dropdown allows users to filter their tasks in the Follow Up Management and Claim sections by Claim Tasks, Follow Up Tasks, or Claim Submission Tasks allowing you to manage all 3 from the same screen. Your task type preferences will then be remembered for each section when opened in the future.
Highlights
| New Features | Enhancements |
|---|---|
| Task Management for Statements New Post Only Payment Permission New Payer-Level Authorization Billing Alert |
AR Aging By Net Amount New Electronic Statements Report Fields |
New features
Task Management for Statement Tracker
As part of our Task workflow improvements project, we added the ability for users to create and manage Patient Tasks based on specific statements within Statement Tracker. Similar to previous enhancements that added tasks to Claim Tracker, Claim Control, and Follow-Up Management, this enhancement allows customers to track statements requiring attention. These tasks include due dates, links, descriptions, statuses, and priorities, and can be assigned to individuals or specific user groups within your organization. Please note that some task management options are exclusive to Plan 3 and above. For more information, visit our Add a Diagnosis Code Help Article

We also added a new "Statement" Task Type that allows users to specifically search for statement tasks. For more information, visit our Statement Tracker Task Options Help Article 
New "Post Only" Payment Permission
Some larger practices or billing services allow certain users to collect patient payments but want to restrict their ability to choose which charges to apply them to. In this release, we added a new “Post Only” level to the existing Patient Payments permission, that will allow the user to post new payments as credits but will prevent them from being able to apply payments, account credits, discounts, or credit/debit adjustments. We also renamed the existing “Allow” level for this permission to “Apply” which will still allow users to post patient payments and apply discounts, credit/debit adjustments, and account credits. 
New Payer-Level Authorization Billing Alert
We previously added code-level authorization alerts to set a prior authorization requirement as a default on the code. On this release, we added the ability to add payer-level authorization alerts, which will help users ensure claims have the proper authorization information before submission. The new Require prior authorization for this payer option will set the requirement for all claims that have that payer set as primary.

When the new payer level option is enabled, a warning will be issued during the claim review since a pre-authorization is required and no authorization number is set on a claim. For more information visit our General Billing Options Help Article. 
Enhancements
AR Aging By Net Amount
We added a new option within the A/R Aging Gadget that allows users to see A/R by Net Amount (expected payment) received from the payer instead of charge amount. This option will show the expected revenue before any insurance adjustments. For more info, visit our AR Aging Gadget Help Article.
Drilling down to the Charge Aging Report from the gadget now also allows you to add columns to your report for Charge Net Amount and Charge Net Balance. 
New Electronic Statements Report Fields
We added 2 new report fields under Patient Data > Electronic Statements for Patient Email Address and Patient Phone Number that allow users to report on where patients are set to receive their electronic statements. Visit our Electronic Statements Report Fields Help Article for more information.
Highlights
| New Features | Enhancements |
|---|---|
| Diagnosis Code Default Procedures New Task Automation For Appointment Cancelation New Basic Appeal & Timely Filing Letters |
Copay Max Increased New Eligibility Report Fields |
New features
Diagnosis Code Default Procedures
We added the ability to automate procedure codes based on diagnosis codes, particularly for diagnoses that consistently require a specific procedure. When set, if a claim is created or a diagnosis code is manually entered, the corresponding procedure code will automatically populate as a charge line item. This new feature allows users to assign up to six default procedure codes per diagnosis code. For more information, visit our Add a Diagnosis Code Help Article

New Task Automation for Appointment Cancellation
We recently added a new Task Automation tab allowing customers to configure their practice to automatically create a new task for any payment failures during the daily AutoPay process. In this release, we are expanding this tab to include a new task automation option to Create a task when a patient cancels their appointment via appointment reminder. When a patient cancels an appointment via an appointment reminder, a user or group can receive an automated task notification, enabling them to immediately fill the slot with another patient. Visit our Task Automations Help Article for more info on setting up this automation. 
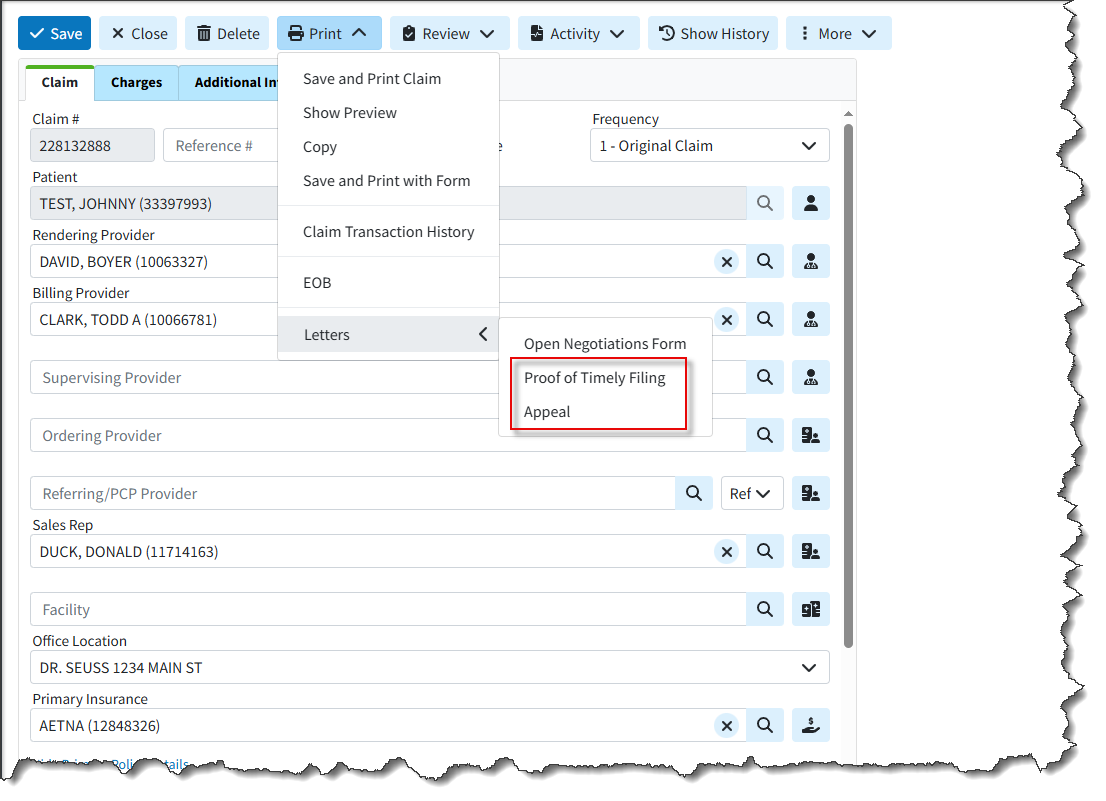
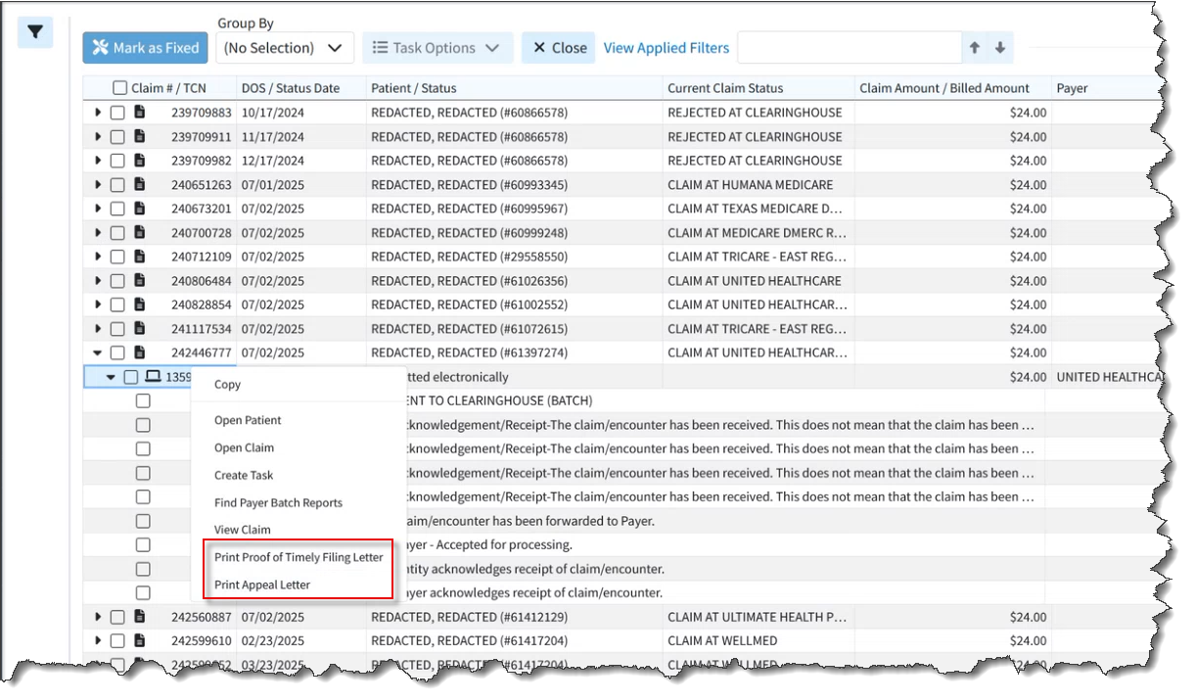
New Basic Appeal & Timely Filing Letters
Previously, users needed to create their own appeal and timely filing letters when they needed to provide those letters to payers. In this release, we added the ability for users to print timely filing and appeal letters directly from the Claim, Claim Tracker, and Claim Follow Up sections of the application. This allows customers to print basic appeal and timely filing letters for payers who don't have their own required format.
Printing Letter From the Claim Section
Printing Letter From the Follow Up Management section

Printing Letter From the Claim Tracker Section
Knowledge base articles
- Print Proof of Timely Filing Letter from Claim Help Article
- Print Appeal Letter From Claim Help Article
- Print Proof of Timely Filing Letter From Follow Up Help Article
- Print Appeal Letter From Follow Up Help Article
- Track a Claim Help Article
- Proof of Timely Filing Letter Sample
- Appeal Letter Sample
Enhancements
Copay Max Increased
As healthcare costs increase, more costs are being shifted to the patient. Previously, the Copay field allowed for up to $999.99, which is generally sufficient for professional services but not for inpatient hospital or maternity copays. (Typically, plans use a coinsurance model for hospital claims, but not all plans do this.) Since the insurance policies table already has a limit of $9,999.99 (based on being a numeric(6,4) column), we expanded the width of the in-app copay fields in the patient section to allow entering values of up to $9,999.99.
New Eligibility Report Fields
In this release, we added the following Eligibility Data report fields for better reporting on Eligibility requests:
- Is Active Coverage? - This field displays if there is active coverage based on the Eligibility.Active field uses Yes or No filter values.
- Message - (text field) This field displays any eligibility messages (error messages).
- Service Type - (filter values are full name) This field displays the service type with values as the full name (i.e., “Medical Care” rather than the code “01”) based on the Eligibility.Servicetype field.
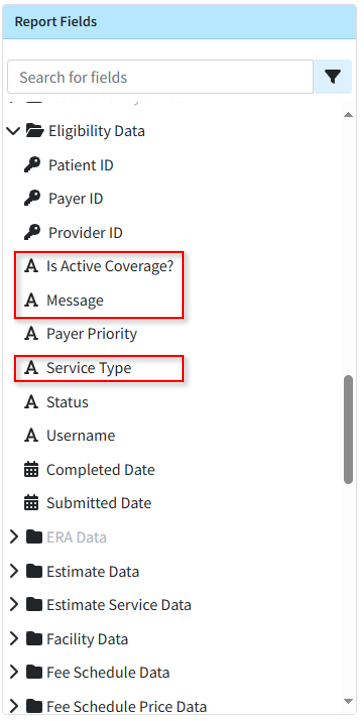
Visit our Eligibility Data Help Article for more information on the new report fields.
Estimates Automation (Charge Detail)
We updated patient estimates for appointments to no longer require re-entering charge details when creating a new estimate for an appointment that already has one. The charge details that were previously entered are now shown by default, eliminating the need for users to re-enter them.
Report Performance Enhancement
We added performance improvements of several reports including the Rev. Claims Billed Charges Report and the Claim Details Report (particularly the Charge Last Billed Date filter) to minimize slowness when running these reports.
Show HL7 Location for Users
A new checkbox was added to the bottom left of the View Message Interface Tracker dialog to display the HL7 location. This checkbox will only be shown for HL7 messages and when checked, the HL7 segment location will be displayed to the user (previously only available with Engineering permissions).
Highlights
| New Features | Enhancements |
|---|---|
| EOB Info Available in Claim & Follow Up Sections |
WebAPI Enhancements |
New features
EOB Information Now Available in Claim & Follow Up Sections
When working claim appeals and denials, users were previously having to juggle multiple windows to see the claim EOB details. In this release, we added a new tab that allows customers to quickly access this information directly within the Claim and Follow Up Management sections so that users can access this information without the need to leave the current screen. The new EOB Info tab is available from the side-panel dropdown (in the Claim and Follow Up sections) and will allow users to view the EOB details including remittance code information. 
To view the EOB details, click the desired check information to open the EOB details window. 
This new tab applies to manually posted insurance payments and applied ERAs. For more info on viewing the EOB Info from a claim or Follow Up, visit our View EOB Info On Claim or View EOB From Follow Up Help Articles.
Enhancements
Web API Enhancements
We added some updates and improvements to the WebAPI so that the following data that was previously only supported either on HL7 or XML is now supported on both.
- Last Menstrual Period: Added Support for receiving the Last Menstrual Period field on inbound claim messages (HL7 claims). This was previously supported only on XML.
- Accident/Illness Date: Added Support for receiving the Accident/Illness Date field on inbound claim messages (XML claims). This vital information for PT and Worker's Comp providers was previously supported only on HL7.
- Race, Ethnicity, Language: Added Support for receiving the Meaningful Use fields for Race, Ethnicity, and Language on inbound claim messages (XML claims). This Meaningful Use information was previously supported on HL7 but undocumented on XML.
Please note that customers need to update the data they send to CMD to take advantage of these new available fields.
We also added a Provider Matching Warning. This means that if a provider name is sent in the interface message and the system selects a provider where the first and last name (or just organization name) is not an exact match, the system will create the claim as usual. However, it will post a Warning message to Interface Tracker stating that the provider was selected based on ID even though the name does not match.
Increased Maximum Length of TCN Prefix
Currently users can enter a TCN Prefix in the Practice section. This is typically done by Support and used by the clearinghouse, but some users may set their own if they do not share an NPI across multiple CMD customers.
Previously, this field was limited to 4 characters. Based on customer requests and considering that our TCNs are 11 characters long and the maximum TCN length in ANSI is 20 characters, we increased the length of the TCN Prefix and Statement TCN Prefix fields to 6 characters. 
Highlights
| New Features | Enhancements |
|---|---|
| Tasks Available in Multiple New Sections New Enhanced Auditing (Show History) for Contracts |
Net Amount now Available in Activity Report Incremental Data Snapshot Option |
New features
Tasks Added to Multiple Sections
We added the ability to add tasks reminders associated with specific records within more sections of the application in order to keep track of items that need to be completed. Tasks can have due dates, links, descriptions, statuses, and priorities. Please be aware that some of these task management options are available in plan 3 and above. You can now assign the following tasks to yourself or to specific users/groups within your business:
Report Snapshot Tasks
A new option was added to create tasks from a Report Snapshot, allowing you to assign a user or group to review specific report results. Creating a task from a report will have the report snapshot linked to it and will be available for 90 days. For more information on saving and creating a task on a report, visit our Create a Task for a Report Help Article

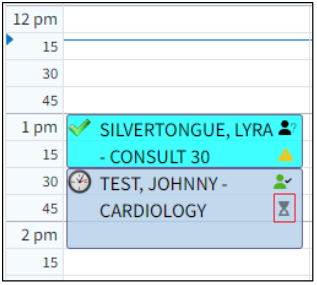
Appointment Tasks
We also added the ability to create and link tasks to specific appointments. Users can access this feature via the right-click menu within the scheduler or the new tasks side panel option. Visit our Appointment Tasks Help Articles for more information on adding and managing appointment tasks.
Tasks From Claim Control
We added new Task Options within the Claim Control screen, allowing users to create and manage tasks associated with specific claims. This new option allows users to create and link tasks to multiple claims at once, as well as reassign and delete them simply by checking them off. For more info on creating tasks from Claim Control, visit our Claim Control Task Options Help Article.
Tasks From Claim Tracker
We also added new Task Options within the Claim Tracker screen, allowing users to create, manage, reassign, and delete tasks associated with specific claims simply by checking them off. Tasks can also be linked to multiple claims simultaneously. Visit our Claim Tracker Task Options Help Article for more information.
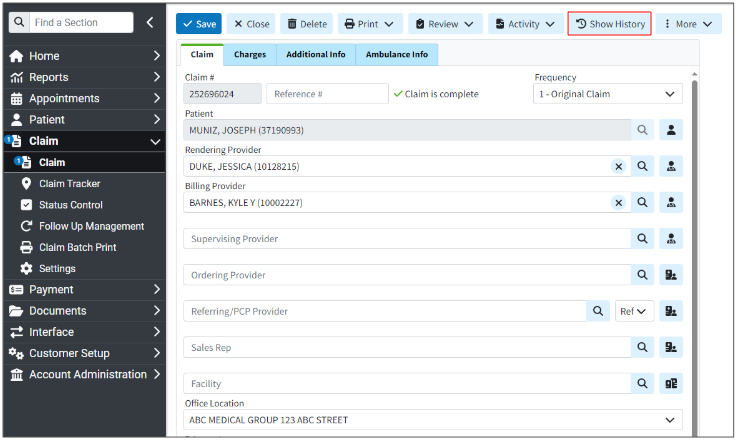
New Enhanced Auditing (Show History) for Contracts
CollaborateMD has been working on a new enhanced auditing project that will provide offices with an easy and transparent way of auditing changes made in the application. We previously released our new Enhanced User Auditing feature in the Customer Setup, Patient, Claim, Appointment, Payment Profiles, Interface Settings, Fee Schedules, and all Customer-level Payment, Claim, and Patient settings sections of the application, allowing users to see a detailed list of changes made to specific records throughout the application.
In this release, we are expanding our Enhanced Auditing functionality to Contracts, enabling users to track modifications, changes, and updates made to contracts for better auditing and accountability. With the new "Show History" feature, you can now determine which user changed/updated a specific contract in the software and when by providing an auditing table with all updates or changes made to a record, including the user, date, time, and the record changed. 
These new auditing records are also included in our existing User Audit Report, making it an even stronger tool for auditing multiple records simultaneously. The Show History capability will be systematically added to other sections of the application. For more information visit our Enhanced Auditing (Show History) Help Article.
Enhancements
Net Amount now Available in Activity Report
We added a new user-level setting to the Patient Settings to display the Net Amount (based on the allowed or contracted amount) in the Patient Activity section. When set to "Yes" (the default is "No"), the Net Amount and Net Balance will be shown in the Claim listing in the Patient Activity. 
This option was added to allow users to view claims on a net basis. When this option is selected, the Balance column will no longer be displayed. Instead, users can utilize the Net Amount and Net Balance columns to see the expected revenue, regardless of whether a contractual adjustment has been entered yet.
For more info on enabling this setting, visit our Configure Patient Settings Help Article.
New Incremental Data Snapshots
In this release, we added a new option for Recurring Data Snapshots to minimize processing time. This option captures only changed items in larger tables, rather than a complete daily database snapshot. When configuring this new "Incremental Snapshot" option, the initial snapshot (or the first snapshot after adding a new customer to a combined snapshot) will be a full snapshot. Subsequent snapshots will export smaller files containing only changed data for Patient, Claim, Charge, Credit, and Activity tables; all other datasets will receive full data. This ensures your snapshot is prioritized and available sooner than full snapshots. Visit our Recurring Data Snapshot Help Article for more info on setting up an Incremental recurring snapshot.
New Aggregation of Text Columns on Reports
We updated the Report Builder to allow aggregations of text columns (in addition to numeric and date) into List, Unique List, Count, and Count Unique. This allows users to create reports detailing payment information, such as a list of payers for a specific claim, a report of all remittance codes, or a summary of distinct check numbers, in order to prevent duplicate lines. 
Highlights
New features
New Claim Workflow Enhancements: Combining Claims
We added a new feature within Claim Control section that allows users to find and combine claims (as long as the claims are for the same patient/payer/provider). CollaborateMD's new Combine Claims feature allows users to merge two or more separate claims into one, consolidating all charges and removing the duplicate claims automatically. This is useful for customers who need to combine encounters into a single claim due to the EHR separating the encounter into multiple claims, payer bundling requirements, or any other reason. Simply select your claims and click the Combine Claims button to start the process. 
You will be presented with a list of charges that will be combined into the new claim where you can reorder the charges before combining them into a new claim. 
Once combined, you can save the new claim, and only the new combined claim will exist, while the individual ones will be deleted. For more information on combining claims, visit our Combine Claims Help Article.
New Claim Workflow Enhancements: New Institutional Defaults
In this release, we have added updates to the patient and payer claim defaults for institutional claims. First, we separated the Patient Claim defaults into Professional and Institutional categories. The availability of Professional or Institutional claim default options depends on whether the default provider for the patient sends professional claims, institutional claims, or both. The claim default options for Professional Claims include ICD and CPT Codes. For Institutional Claims, the options are Principal Diagnosis, POA, Other Diagnosis, CPT Codes, and Value Codes to provide more flexibility when setting your defaults. For more information on setting up institutional patient claim defaults, visit our Patient Claim Defaults Help Article. We also added 2 payer billing options for claims. Within the General Billing Options tab, we introduced a new option to select a Default Value Code to be included on institutional claims for this payer. Additionally, under the Provider Billing Options, we added an option to select a Default Referring Provider for every claim under this provider. Visit our General Billing Options and Provider Billing Options Help Articles for more information.
We also added 2 payer billing options for claims. Within the General Billing Options tab, we introduced a new option to select a Default Value Code to be included on institutional claims for this payer. Additionally, under the Provider Billing Options, we added an option to select a Default Referring Provider for every claim under this provider. Visit our General Billing Options and Provider Billing Options Help Articles for more information.
New Task Automation for AutoPay
We added a new Task Automation feature allowing customers to configure their practice to automatically create a new task for any payment failures during the daily AutoPay process. This task will be linked to the patient and assigned to a pre-selected user or group. Customers that use the AutoPay feature can now set up the "Create a task when a patient's AutoPay payment fails" task automation from the practices right-hand side panel. Visit our Task Automations Help Article for more info on setting up this automation. 
Custom Claim Scrubbing Edits & Claim Scrubbing Specialty
In this release, we added two significant enhancements to our Claim Scrubbing. First, we introduced an option within the Claim Scrubbing configuration screen that allows customers to set up (or change) their specialty to receive more tailored edits for their specific claims. Visit our Manage Claim Scrubbing Help Article for more information on setting your Specialty. Secondly, we introduced a new Claim Scrubbing Custom Edits & Analytics service that provides customers access to the ClaimStaker® application, allowing them to review existing claim scrubbing edits, create new ones, and review detailed analytics. This is a paid service that can be requested from Services > Other Services and includes one initial training session on how to use ClaimStaker® to create custom edits and review analytics.
Secondly, we introduced a new Claim Scrubbing Custom Edits & Analytics service that provides customers access to the ClaimStaker® application, allowing them to review existing claim scrubbing edits, create new ones, and review detailed analytics. This is a paid service that can be requested from Services > Other Services and includes one initial training session on how to use ClaimStaker® to create custom edits and review analytics. 
For more information on requesting this service, visit our Request Claim Scrubbing Custom Edits & Analytics Help Article.
Enhancements
New Claim Workflow Enhancements: New Situational Modifier Options
In this release, we have added a couple of updates to the situational modifiers for procedure codes. First, we introduced two new options within the Procedure Codes to set Situational Modifiers.
- A new option to create a situational modifier based on "A specific type of service" to set a specific TOS code that the modifier should apply to.
A new option to create a situational modifier based on "A specific other procedure code on the claim" to select a procedure code that will trigger the modifier only when this other procedure is present on a claim.
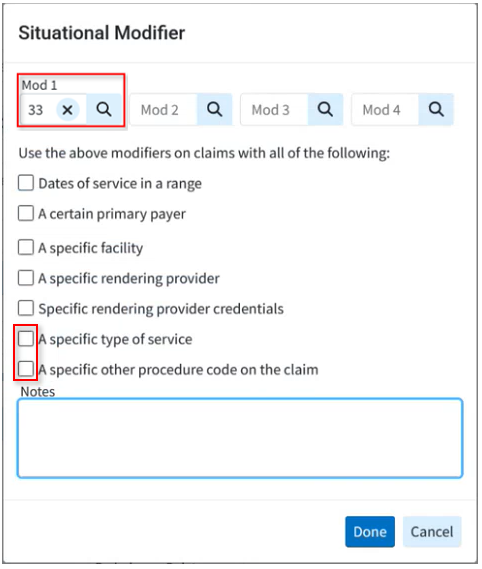
We also updated the Dates of Service, Primary Payer, Facility, Rendering Provider, Rendering Provider Credentials, and TOS situational modifier options to be multi-select, making it easier for practices with a large number of records to manage these modifiers. For more information on adding these modifiers, visit our Add Situational Modifiers Help Article.
New Claim Workflow Enhancements: Claim Status Updates
We updated our Real-Time Claim Status results window to allow users to update the claim charge status directly from the results screen. Users can now also enter any follow-up notes pertaining to the claim, as well as any expected payment information from the status result (paid amount, check date, and check number). This update will automatically override any existing data in Expected Payment Info with information from the Claim Status if the payer made a payment. For more information visit our Claim Status Help Article.
Highlights
| New Features | Enhancements |
|---|---|
| New Task Assignment to Contact Groups
New Prior Auth Requirement & Billing Alerts Update New Appointment Types Default Codes |
New Taxonomy Specialty Report Fields |
New features
New Task Assignment to Contact Groups
Capitalizing on our recently released Shared Contact Groups feature, users can now assign tasks to individuals within a Contact Group. You can create Contact Groups for teams (denials, billing, specific offices, payments, etc.) and assign tasks to those groups to ensure work is completed. All users in the group will see the tasks assigned to the group, and once completed, the system will track which user completed the task via the User Productivity by Tasks Completed Report, allowing you to monitor user productivity. For more information creating Shared contact groups, visit our Create a Shared Contact Group Help Article. For info on assigning tasks to a contact group, visit our Assign a Task to a Contact Group Help Article.
New Prior Authorization Requirements & Billing Alerts Update
In this release, we have added a couple of updates to the billing alerts for procedure codes. First, we introduced a new option within the Procedure Codes setup window to set a Prior Authorization Requirement as a default on the code. You can set the Prior Authorization Requirement on a code for all payers or a list of specific payers. When there is a pre-authorization requirement and no authorization number is set on a claim, you will now receive a warning during the claim review. For more information on setting up a prior authorization requirement, visit our Add CPT/HCPCS Codes Help Article.
We also updated the placement of billing alert warnings within the application. Billing alerts will now be displayed not only in the claim section, but also in the claim control area when running the claim review process. This change is intended to help our interface customers more easily access these billing alerts, as they are now integrated into the claim review workflow.
New Appointment Type Default Codes
We previously added claim defaults for POS and TOS within the Appointment Types configuration. In this release, we introduced Appointment Type Default Codes, allowing users to set default procedure codes on appointment types. When creating claims from the appointment scheduler, these default codes will be used. New estimates created from the appointment scheduler will also use default procedures from the Appointment Type, making estimates faster and easier than ever.
Please note that these default codes apply only to claims created from an appointment. Patient Default Procedure Codes won't be used if the Appointment Type has a default procedure, though patient default diagnosis codes will still be used. Claims created from the claim section will not use these Appointment Type default codes, only Patient Defaults if available. Visit our Add New Appointment Type Help Article for more info on adding default codes to an Appointment Type. 
Enhancements
New Report Fields
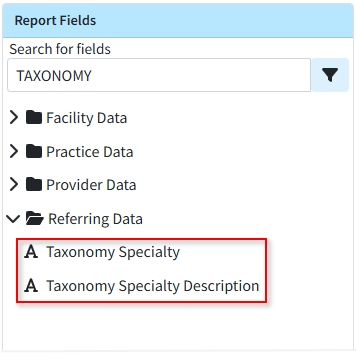
Previously, users could add fields related to the taxonomy specialty and the taxonomy specialty description for Providers and Practice, but not for Referring Providers. In this release, we added fields to report on taxonomy codes (specialties) and its description for Referring Providers.- Referring Data → Taxonomy Specialty
- Referring Data → Taxonomy Specialty Description
View Prior Claim Status Checks
We have long supported viewing prior claim status checks from the Claim section, but this ability was not available for claim follow-ups. In this release, we added this capability to the Claim Follow-Up Management section.
Web API Updates
In this release, we made a few enhancements to our WebAPI. On professional claims, we support the "Charge To Date" to represent charges over a period of time. This "to date of service" can be sent in the FT1.5 segment. However, on institutional claims, there is no location on the claim form for the "To Date of Service" for any particular charge, so we do not support it. Since some payers require sending one charge with multiple units to cover multiple days, and individual charges are the only way to send dates, and institutional claims don’t support the "To Date of Service," it becomes difficult to set a "Statement Covers To" date that extends beyond the last charge’s date of service. In this release, we updated our WebAPI to internally store a "To Date" of service and use it to determine the claim's statement covers "To" and "From" dates when a single charge covers multiple days.
We also added the ability to add payments via the WebAPI. Previously, when we received payments from the WebAPI, they were applied as a credit, and users had to access the application to apply the payment. In this release, we updated the WebAPI to allow users to apply a patient payment directly to specific claims instead of as a credit. Users can now use the Activity or Charge History APIs to get charge details and use that information to choose where to apply new payments (only new payments, not existing credits).
Resolutions
ERA Secondary OA-23 Adjustments Update
The process of applying a secondary adjustment on an ERA has been updated to no longer allow the OA-23 adjustment. This adjustment, related to prior payers' payments and adjustments, should never be applied as it can incorrectly affect the balance and cause an incorrect account credit.
Update from Release 15.9 (Net Amount available in the Activity Report)
We recently added a new user-level setting to the Patient Settings to display the Net Amount (based on the allowed or contracted amount) in the Patient Activity section. When set to "Yes," the Net Amount and Net Balance would be shown in the Claim listing in the Patient Activity. In this release, we removed this setting due to an issue found with the feature. We will correct this and re-release it in the June-July timeframe.
Highlights
| New Features | Enhancements |
|---|---|
| New Split Claim Feature Enhanced Auditing for Fee Schedules & Customer-level Settings |
A/R Control Payer Filter Renamed |
New features
New Split Claim Feature
There are certain scenarios where claims need to be split. This could occur when an interface sends a single visit that should have been billed as multiple claims, or when a secondary payer has different bundling requirements than the primary payer. In these cases, users previously had to delete and re-enter payments or completely recreate the claim and duplicate the payments. To streamline this process, we released a new Split Claim feature that allows users to take a single claim and quickly split it into multiple claims. This option within the More menu in a claim enables users to move selected charges, including any existing payments, to a new claim, saving a significant amount of time. 
This new option allows users to select which charges will transfer to the new claim simply by checking them. Once moved, any associated payment history is automatically transferred, even if the claim has already been submitted. Please note that you are only able to split one claim into two. If you wish to split it further, you can reopen the claim after splitting it once.

Knowledge base articles
New Enhanced Auditing (Show History) for Fee Schedules & Customer-level Settings
CollaborateMD has been working on a new enhanced auditing project that will provide offices with an easy and transparent way of auditing changes made in the application. We previously released our new Enhanced User Auditing feature in the Customer Setup, Patient, Claim, Appointment, Payment Profiles, and Interface Settings sections of the application, allowing users to see a detailed list of changes made to specific records throughout the application.
In this release, we are expanding our Enhanced Auditing functionality to the Fee Schedules and all Customer-level Payment, Claim, and Patient settings, enabling users to track modifications, changes, and updates made to fee schedules and settings for better auditing and accountability. With the new "Show History" feature, you can now determine which user changed/updated a specific setting or fee schedule in the software and when by providing an auditing table with all updates or changes made to a record, including the user, date, time, and the record changed. 
These new auditing records are also included in our existing User Audit Report, making it an even stronger tool for auditing multiple records simultaneously. The Show History capability has currently been deployed in the Customer Setup, Patient, Claim, Appointments, Payment Profiles, Interface Settings, Fee Schedules, and Customer-level Setting sections, and we will be systematically adding it to other sections of the application.
Knowledge base articles
Enhancements
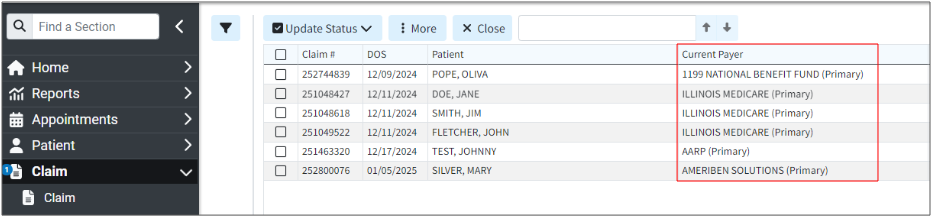
A/R Control Payer Filter Renamed
Previously, the existing A/R Control "Payer" filter could potentially confuse users who might expect it to "show any claims with this payer on it" instead of "showing claims currently at this payer," which is what it actually checks. In this release, we updated the filter name from "Payer" to "Current Payer" to better reflect its actual use. Please note that only the name has changed; the filter itself remains the same.
Knowledge base articles
Resolutions
ERA Contract Updates
When a contract warning appears in the ERA section, we will no longer allow users to update the contract from the ERA warning if the allowed amount is $0.00. Previously, this could allow users to incorrectly update their contracts based on a $0.00 allowed amount, when it was actually a claim denial or rejection and not a reflection of a contract needing to be updated. The warning itself, if your contract amount doesn't match the allowed amount, will still show (alongside informational items stating that the payer did not pay); however, the system will not allow you to update the contract directly from the warning.
Highlights
| New Features | Enhancements |
|---|---|
| New Re-Order charges on claims option Enhanced Auditing for Payment Profiles & Interface Settings |
New Shared Contact Groups |
New features
New claim option to Re-Order charges
We added a new option that allows customers to quickly reorder charges on claims without completely re-entering them. This new column enables customers to change the order of charges on a claim in seconds for payers with specific requirements, even between primary and secondary payers. With this new drag-and-drop option, it's never been easier to change the order of charges on claims. 
Knowledge base articles
New Enhanced Auditing (Show History) for Payment Profiles & Interface Settings
CollaborateMD has been working on a new enhanced auditing project that will provide offices with an easy and transparent way of auditing changes made in the application. We previously released our new Enhanced User Auditing feature in the Customer Setup, Patient, Claim, and Appointment sections of the application, allowing users to see a detailed list of changes made to specific records throughout the application.
In this release, we are expanding our Enhanced Auditing functionality to the Payment Profiles and Interface Settings, enabling users to track modifications, changes, and updates made to these 2 sections within CMD for better auditing and accountability. With the new "Show History" feature, you can now determine which user changed/updated a specific payment profile or interface setting in the software and when by providing an auditing table with all updates or changes made to a record, including the user, date, time, and the record changed. 
Please note that when auditing changes to a payment profile's credit card #, only the first and the last digits of the card will be visible. These new auditing records are also included in our existing User Audit Report, making it an even stronger tool for auditing multiple records simultaneously. The Show History capability has currently been deployed in the Customer Setup, Patient, Claim, Appointments, Payment Profiles, and Interface Settings sections, and we will be systematically adding it to other sections of the application.
Knowledge base articles
Enhancements
New Shared Contact Groups
We added a Shared Contact Groups option within CMD Messaging, enabling users to send messages to groups and share those groups across their organization. This new option is controlled by an additional permission level within the existing Contacts permission. It allows users to create and share contact groups for those employees working on specific tasks (e.g., denials or collections) to ensure timely notifications are sent to the appropriate individuals. 
Knowledge base articles
Resolutions
Text not highlighted within tables when a field was selected
Corrected a minor visual issue that prevented text from being highlighted in tables for some Chrome users when an input field was selected. This affected all sections but did not impact keyboard functionality when typing to replace content in the field. 
New features | Enhancements | Resolutions
New features
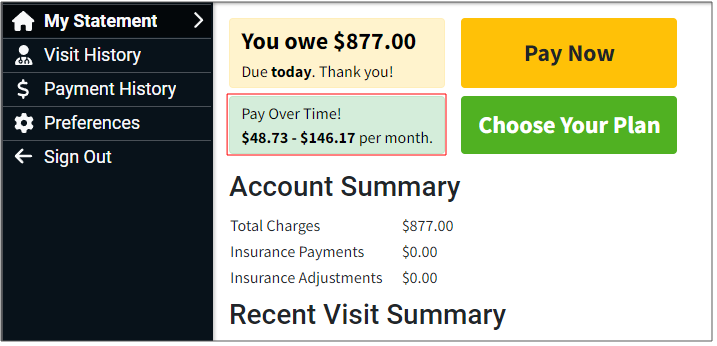
New Pay Over Time with Sunbit feature integration
CollaborateMD now has an integrated partnership with Sunbit's buy now, pay later (BNPL) technology. Trusted healthcare practices and medical billing platforms can now choose Sunbit as a patient-friendly solution for post-care payment plans. Sunbit helps eliminate the stress of managing in-house payment plans by offering a pay-over-time option for patient invoices.
Providers can now offer their patients financing without assuming any financial risk themselves, as they receive the full amount within a few days. Sunbit manages all patient billing, enabling providers to reduce time in accounts receivable and minimize effort on collections. Patients can easily request financing directly from the payment portal, benefiting from a 90% approval rate and a 0% financing option for 3 months. Additionally, there are 6, 12, and 18-month plans with competitive interest rates.
Important Note: You must have the In-App Credit Card Processing and the Patient Payment Portal features enabled and configured so your patients can use Pay Over Time with Sunbit from the portal. 
Knowledge base articles
- Pay Over Time with Sunbit
- Manage Pay Over Time with Sunbit
- Create a Payment Plan with Sunbit
- Refund a Sunbit (Pay Over Time) Patient Payment
- Merchant Payments Report
- Manage your Patient Payment Portal
New Clinical Laboratory Fee Schedule
We added the Centers for Medicare and Medicaid Services (CMS) "Clinical Laboratory Fee Schedule" for customers who are not physicians or who perform services not covered by the Medicare Physician Fee Schedule but can still be paid by Medicare. Lab customers or any customer who orders lab tests can now take advantage of fee schedules and contracts based on the Medicare Clinical Laboratory Fee Schedule (CLFS). When creating a fee schedule or contract using the Medicare Fee Schedule in CMD, it will include the Medicare Physician Fee Schedule and the Medicare Clinical Laboratory Fee Schedule. The Clinical Laboratory Fee Schedule will price procedure codes associated with a lab or test, while the Medicare Physician Fee Schedule will price other procedures.
The Medicare Clinical Laboratory Fee Schedule will be updated quarterly and consists of a single price, either local or national, in contrast to the Medicare Physician Fee Schedule, which is determined based on the specific ZIP code location. 
Knowledge base articles
New Payer Agreement Signature option
We added a new feature for completing payer agreements that require a physical signature but allow for electronic submission of the agreement with the wet signature. This option enables the provider to print, sign, and scan the form, then upload the scanned PDF within the application as part of the Submit Facility NPI Enrollment Form API, similar to the electronic signature process. 
Knowledge base articles
Enhancements
New 0ption to allow sending Clearinghouse Notifications via email
Previously, clearinghouse notifications could only be subscribed to using the CMD Messaging option. In this release, we added the ability to receive Clearinghouse notifications via email, in addition to CMD Messaging. The default will remain CMD Messaging, but users can now configure Clearinghouse notifications to be sent via email within their User Profile > Communication Preferences. 
Knowledge base articles
New 0ption to set non-all-inclusive charges as Paid after billing
We recently added a new feature to the Codes section that allows users to bill other charges when there is an "all-inclusive" charge on the claim, while still sending other charges as $0.00 or $0.01. These charges are then sent as information to the payer but will not be paid. Users would then need to manually adjust, delete, or mark these charges as paid, which created extra work. In this release, we introduced a new option on the Procedure Codes screen to automatically set non-all-inclusive charges as paid after billing. After selecting one of the options to send all other charges on the claim as $0.00 or $0.01, you can choose to automatically mark the other charges as paid after billing, which will set all other charges to PAID rather than AT INSURANCE when claims are submitted. 
Knowledge base articles
New "Current Status" column on EOB/ERA
When posting an insurance payment (manual or ERA) and viewing an individual EOB, the current claim status (not the status that will be set when the payment is posted) is available when hovering over the Status column. In this release, we added a new optional column, hidden by default, to the individual EOB screen. The new "Current Status" column will show the current claim status for better visibility in some workflows. 
New Search option when searching in specific dropdown select fields
We added the ability to search and filter dropdowns with a visual confirmation when typing or searching in the Charge Status, Account Type, and Eligibility Service Type dropdown fields so users can see when they search for dropdown items. 
Resolutions
The "Close and Open Claim" option is missing from Patient > View All Claims
Corrected an issue preventing users from opening a claim from Patient > More > View All Claims when a claim is already open. We previously added this prompt to other sections where claims could be opened, allowing the user to open the claim in a new tab or close the existing claim and open a new one from the prompt. In this release, we updated this screen to prompt the user to close the current claim before opening a new one, as it does on other screens. 
Enhancements
Enhancements
Provider Adjustments Details screen update
Updated the Help Text for the Provider Adjustment Details screen at the top to include links pointing directly to help pages that will aid customers in understanding what provider-level adjustments are and how to post them. The text will now provide a brief description of what provider adjustments are and include links to help articles on associating and applying provider adjustments on claims, as well as automatically posting interest amounts as payments. 
Knowledge base articles
Referring Provider filter updated in multiple locations
The Referring Provider filter has been modified to function as a search field instead of a dropdown menu when the number of referring providers exceeds 20. This change aligns the behavior of the Referring Provider filter with that of the Rendering Provider and Payer search fields across the Control, Tracking, and Batch sections of the application. This search field offers enhanced searching and improved performance for accounts with more than 20 referring providers while maintaining the simplicity of a dropdown menu for customers with fewer than 20. 
New Features and Updates
General
Appointments
- New Enhanced Auditing (Show History) for Appointments: CollaborateMD has been working on a new enhanced auditing project that will provide offices with an easy and transparent way of auditing changes made in the application. We previously released our new Enhanced User Auditing feature in the Customer Setup, Patient, and Claim sections of the application, allowing users to see a detailed list of changes made to specific records throughout the application.
In this release, we are expanding our Enhanced Auditing functionality to the Appointments section, enabling users to track modifications, changes, and updates made to appointments within CMD for better auditing and accountability. With the new "Show History" feature, you can now determine which user changed/updated specific appointment information in the software and when by providing an auditing table with all updates or changes made to a record, including the user, date and time, and the record changed. 
These new auditing records are also included in our existing User Audit Report, making it an even stronger tool for auditing multiple records simultaneously. The Show History capability has currently been deployed in the Customer Setup, Patient, Claim, and Appointments sections, and we will be systematically adding it to other sections of the application.
For more information on using our new Add New Same/Similar Code List feature, please visit our Enhanced Auditing Help Articles.
New Features and Updates
General
Claims
- New Mass Claim Updates Feature: CollaborateMD has always provided powerful tools for working with individual claims, but the platform's ability to make changes to multiple claims at once was limited. With this release, users no longer have to open each claim individually when correcting minor mistakes, such as setting the wrong rendering provider or place of service code on claims. We added a new Mass Claim Updates feature that enhances the existing Status Control screen with capabilities to modify multiple claims. The Status Control screen has been renamed Claim Control, where users can now manage the review of incoming claims from their EHR, submit or resubmit claims, and make updates to multiple claims at once, such as updating the Rendering and Billing Providers, the Facility, the Office Location, or the Place of Service by simply selecting the claim(s) and choosing the Update Claims option.
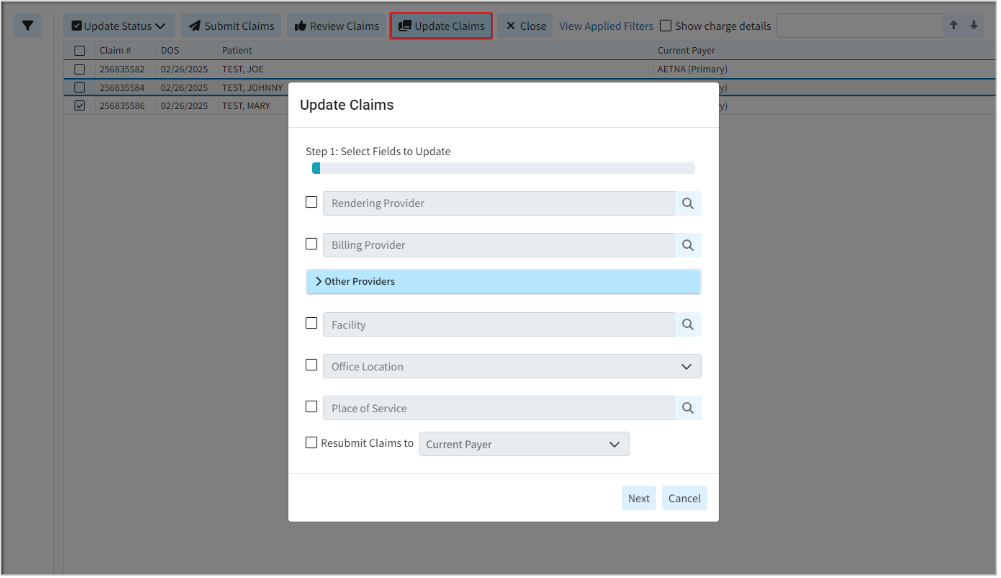
For more information on updating multiple claims at once, please visit our Update Multiple Claims Help Article.
-
Alternate Option To Open A Claim In a Separate Tab When Another Claim Is Already Open: We have introduced a new dialog box option that appears when a user attempts to open a claim from any section within the CMD while a claim is already open. This feature will now provide the user with the following options:
- Close and Open - Closes the open claim and opens a new one (it will display the usual unsaved changes warning and allow the user to save if there are unsaved changes).
- Open in New Tab - Opens a new window/tab with the correct URL/claim
- Cancel - Closes the dialog and keeps the claim open.
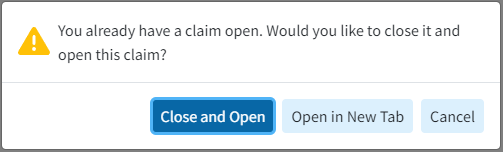
Reports
- Update to the Report Builder to Prevent the "Claim Last Billed Date" Field from Being Added as a Filter: Updated the Report Builder to prevent adding the "Claim Last Billed Date" report field as a Report Filter. While some customers may still try using this field as a filter, we've added a warning message directing them to use the "Charge Last Billed Date" instead, which provides the same results, is much faster, and can potentially be improved further via an index.
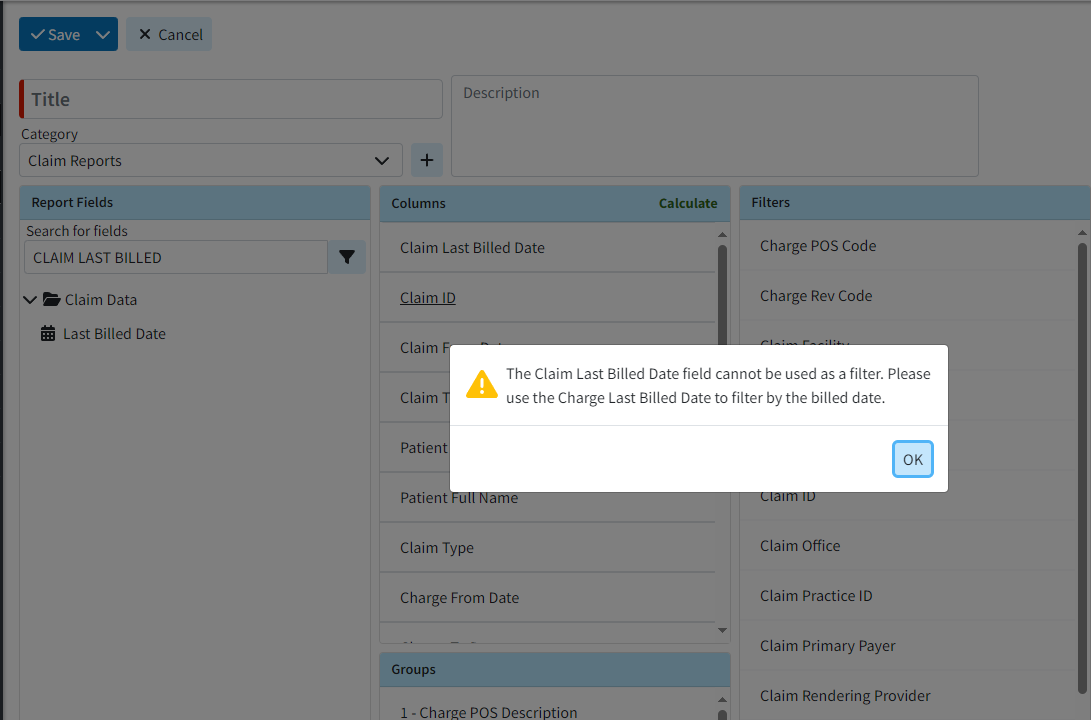
Patient
- New Appointment View Option From The Patient Section: Previously, the "View All Appointments" button directed users to the Appointment section to view a patient's appointment details, requiring them to leave the current section even if they only needed the dates of past appointments. In this release, we added a new "Appointments" option in the patient side panel that displays a list of all appointments (categorized into Past Appointments and Future Appointments) for the patient without leaving the screen. The section will still provide an option for users to access the "View All Appointments" button, directing them to the Appointment section where they can see patient appointment details.
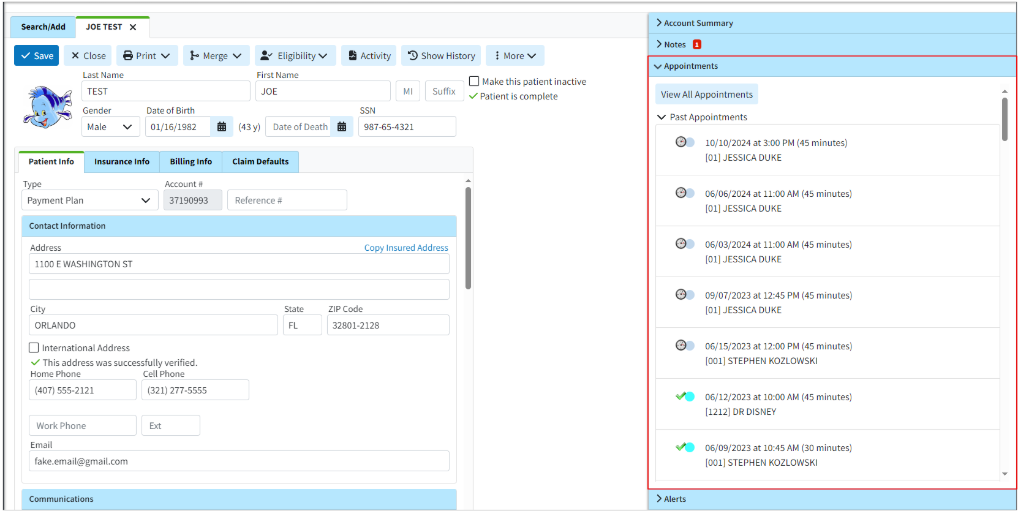
For more information on our new Appointments dropdown, please visit our View Appointments From Patient Section Help Articles.
Customer Setup
- New Option to Open Contracts and Fee Schedules From Procedure & Revenue Codes Section: We added the ability for users to open contracts and fee schedules directly from the Procedure and Revenue Codes sections. This new functionality enables users to click on the Fee Schedule/Contract Name (which is now a clickable link) within the Contracts and Fee Schedules side panel, allowing them to access and view the associated contracts and fee schedules.
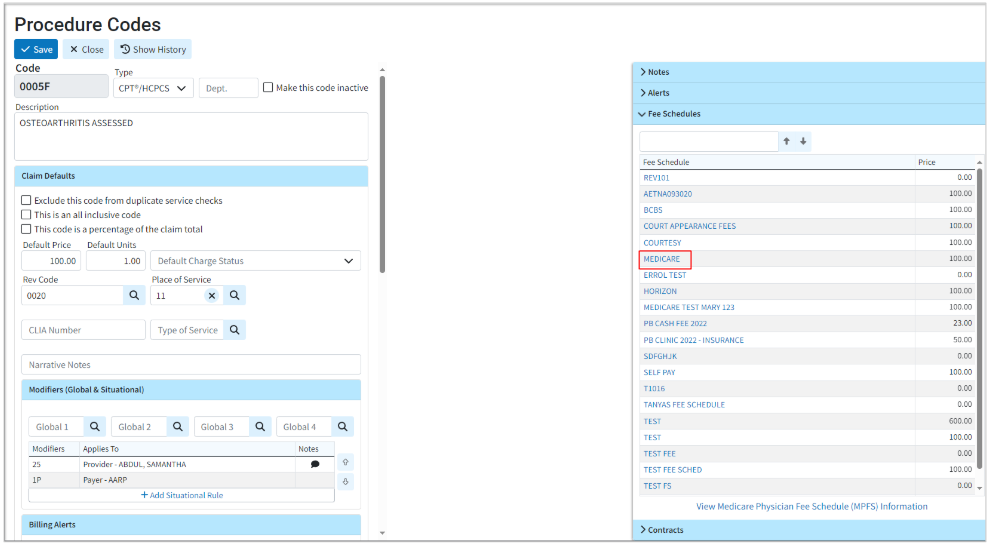
For more information on accessing fee schedules/Contracts from procedure codes, please visit our Procedure Codes Fee Schedules or Procedure Codes Contract Help Articles. For information on accessing fee schedules/Contracts from revenue codes, please visit our Revenue Codes Fee Schedules or Revenue Codes Contract Help Articles.
User Profile
- New Email Option For Two-Factor Authentication: We updated our Two-Factor Authentication to now support email authentication. This option will send an email message with a 6-digit login code, similar to the SMS verification, and can only be set up with the email attached to the user's CMD profile. Please note that if an email address is used that does not match the one set in your user profile, you will receive a warning.
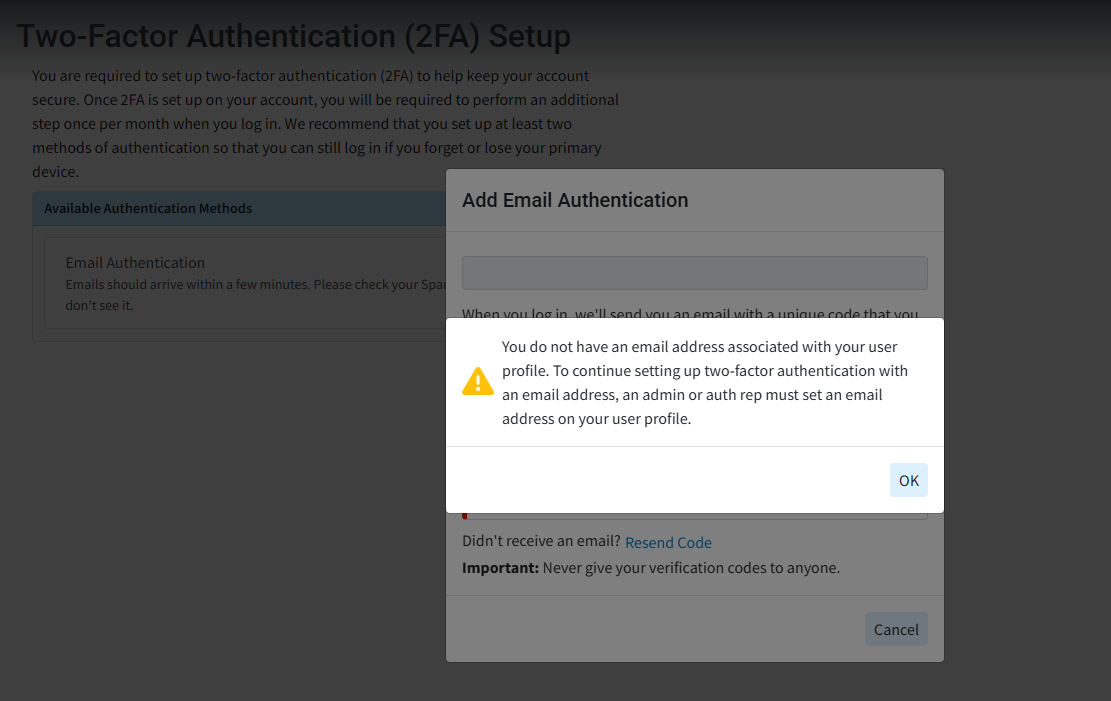
New Features and Updates
General
Patient
- New Balance Due Insurance Optional Column: Some healthcare providers rarely bill patients directly, instead focusing primarily on the balance owed by insurance companies rather than the patient's balance. The patient search screen (results dialog) already displayed the balance owed by insurance, but this information was not shown in the recently opened table. In this release, We added the Balance Due Insurance as an optional column (hidden by default) within the Patient Search screen's Recently Opened list.
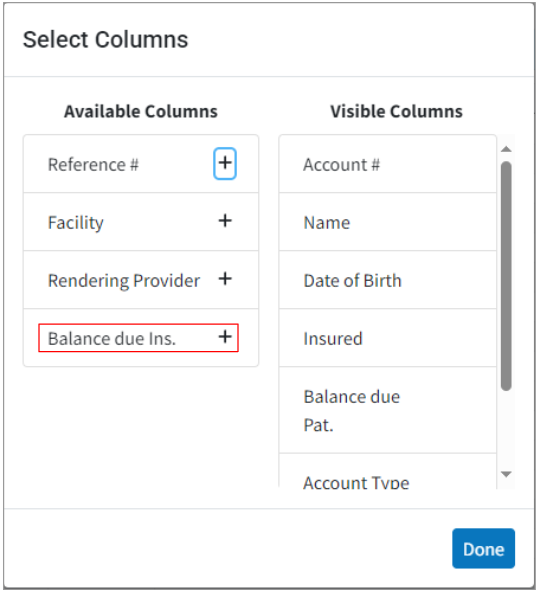
-
New A/R Control Filters Related To Payment Portal Invites: We recently added an option to Send Payment Portal Invites as a batch action from Patient A/R Control. In this release, we added new filters within A/R Control to determine whether or not a patient has enrolled with the payment portal. Customers can now search by a new Date Search Option "Days Since Last Payment Portal Invite Sent," or by the Claim Search Option "Payment Portal Status" (Invitation Not Sent, Invitation Sent but Not Registered, Registered).
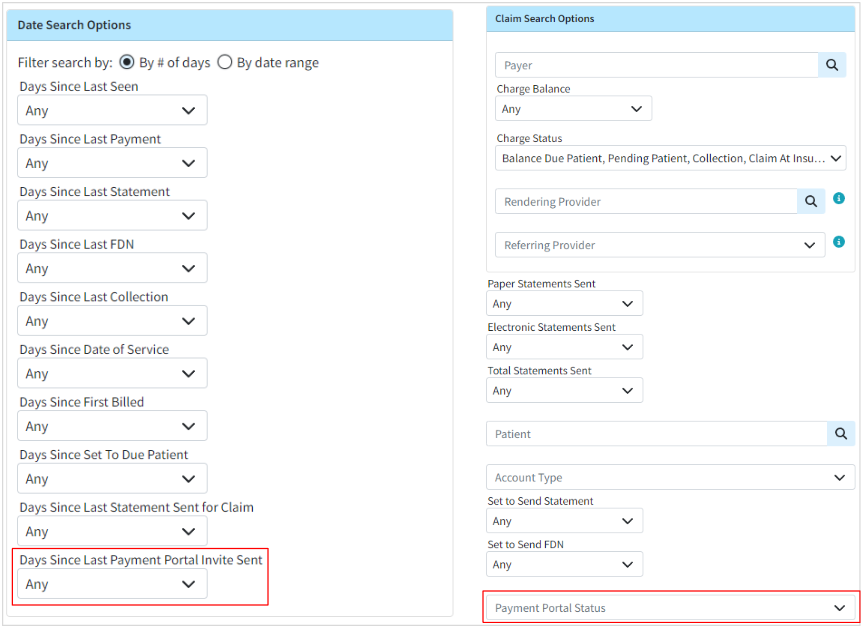 For more information on determining if patients have enrolled in the payment portal, please visit our Search For Patient Balances Help Article.
For more information on determining if patients have enrolled in the payment portal, please visit our Search For Patient Balances Help Article.
Claim
- Updated the Claim Search Capability: When users receive communication from the payer about a claim, it often includes the payer’s claim number: the ICN (Internal Control Number), Claim Control Number, or Original Reference #. These numbers are automatically populated on the claim after the ERA is applied, so the ability to find claims by the ICN is a great tool to have when working on appeals. In this release, we updated the Claim Search capability to include searching by all three claim control numbers, making it easier to locate specific claims during the appeals process.
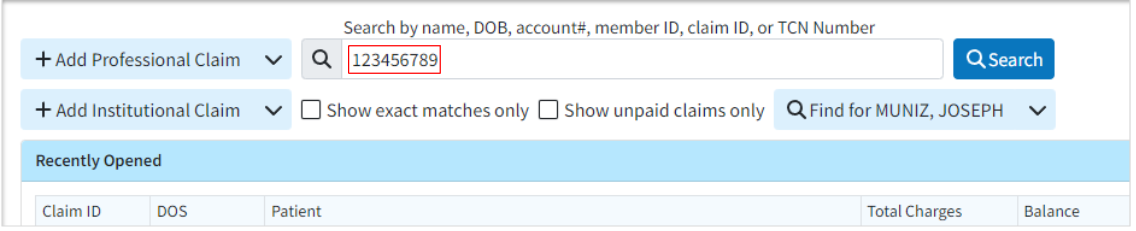
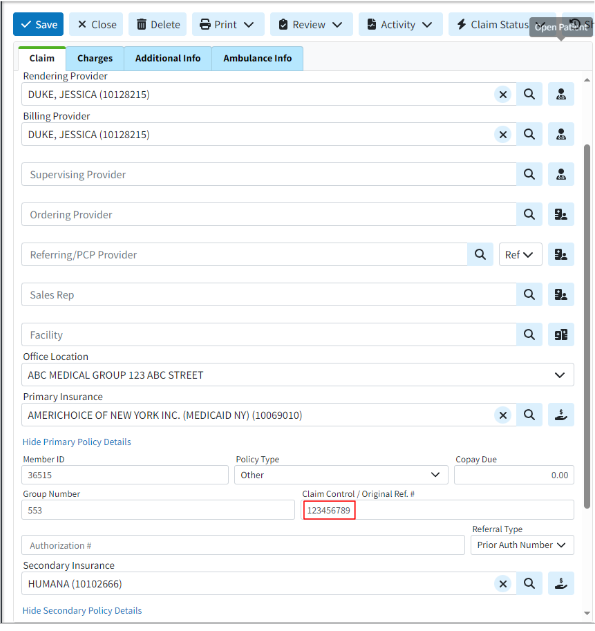
- New Optional Column For Document Count: We added a new optional column (hidden by default) to the Claim, Patient, and Payment sections that display a count of the documents associated with each item. This column helps indicate if a patient, claim, or payment has a document association before opening it.
Please note that this column option will only appear on the search screen after a search is performed, not on the Recently Opened List.
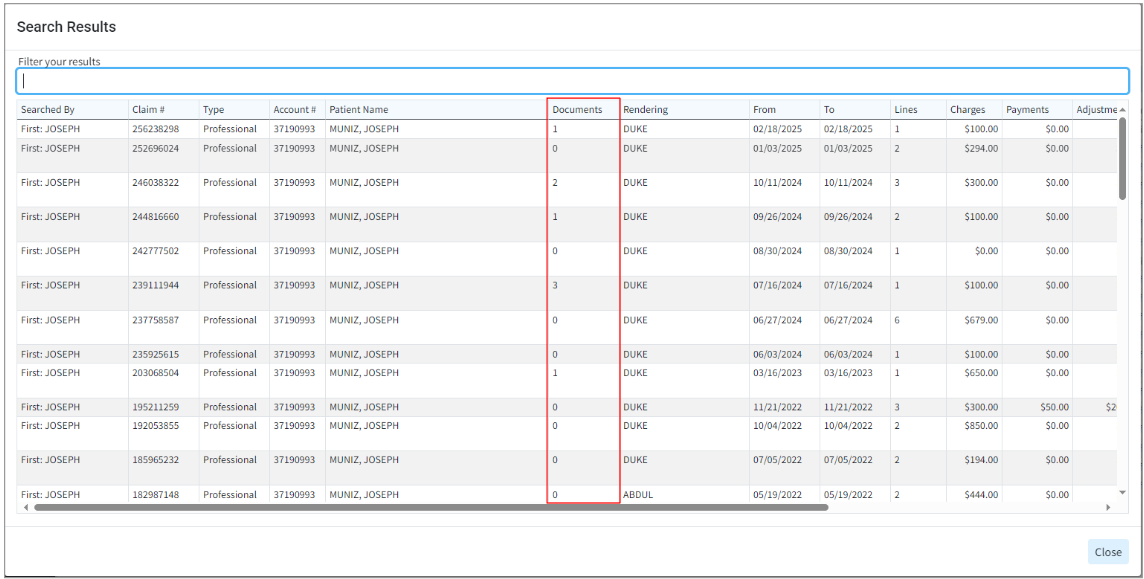
Payment
- Updated The Refund Receipts: Previously, when refund receipts were generated, they appeared identical to a standard receipt, except that the refund amount was displayed within parentheses. To make these receipts more easily identifiable and comprehensible, we modified the refund receipt by adding the word "Refund" to the text and displaying negative numbers with a negative symbol instead of using parentheses, making it clearer.
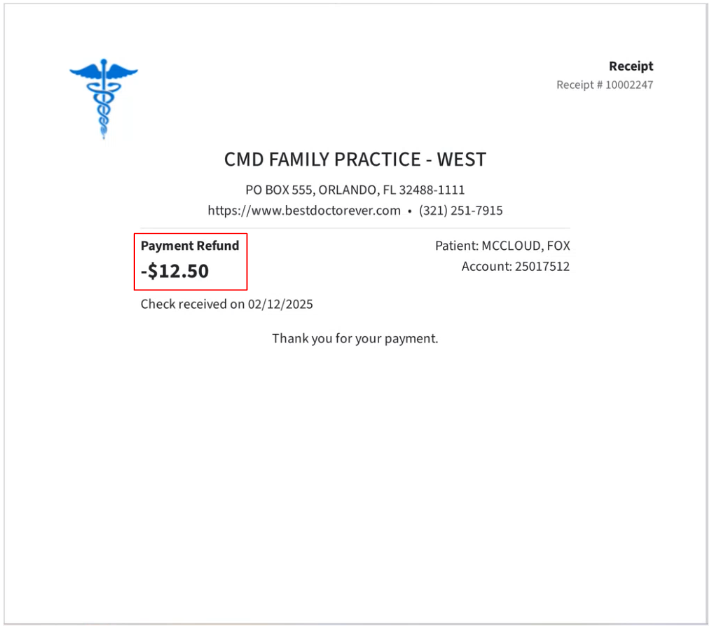
New Features and Updates
General
Appointments
- New Appointment Setting to Hide The Status of Received/Applied Intake Forms: Some users who have tightly packed schedules (double/triple booked) may struggle to see the specifics of their appointments due to the two types of icons we show (the eligibility icon and the forms icon) taking up a lot of the appointment space. To help with this, we introduced a setting that allows users to hide the checkmark that indicates forms that have been submitted.
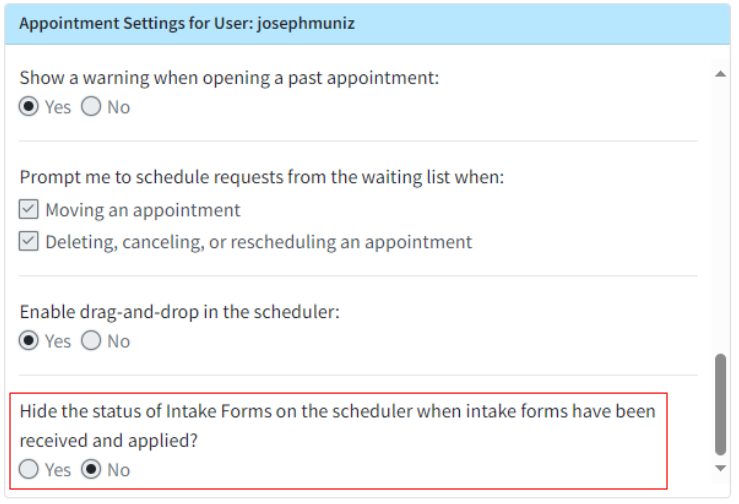
Visit our Configure User Appointment Settings Help Articles for more information on how to turn on this setting.
Patient
- New Patient Broadcast Communications Feature: Patient engagement is the collaborative process between healthcare providers and patients aimed at improving patient health. Over the past few years, the significance and prevalence of patient engagement have grown considerably. Research indicates that when patients feel involved and take an active role in their medical care, they achieve improved health results. Simultaneously, providers observe increased patient satisfaction and retention.
In order to meet the growing needs of both providers and patients, CollaborateMD has developed and introduced a new Patient Broadcast Communications feature. This feature allows providers to send targeted one-way communications to multiple patients using various methods (text, email, or phone). Customers can set campaigns with customized parameters to target specific patients, helping them with their healthcare needs and encouraging retention or usage of optional/elective medical services through intelligent marketing.
For more information on using our new Patient Broadcast Communications feature, please visit our Broadcast Communications Help Articles. For instructions on how to enable and configure the feature, visit our Manage Broadcast Communications Help Article.
- New A/R Control Filters: Some of our customers have very particular workflows and have requested to be able to search in A/R Control by Referring and Rendering providers. This would enable them to send out statements only for claims from a particular provider. To address this need, we added the ability to filter by Rendering or Referring Provider within A/R Control, allowing customers to send statements only for claims from a specific provider or referrer. These new filter options were added under a new header within the A/R Control Filters called "Claim Search Options." Additionally, the existing Payer, Charge Balance, and Charge Status filters have been moved under the Claim Search Options.
For more information on these new filters, please visit our Search For Patient Balances Help Article.
Reports
- New Report Fields For Contract Name: We previously had a number of fields that could be used to show the contract price that applies to a charge. In this release, we added "Contract Name" as a report field under those same data sections . This new field is available under Charge/Debit Data > Charges > Current Payer (as well as Primary/Secondary/Tertiary Payers).
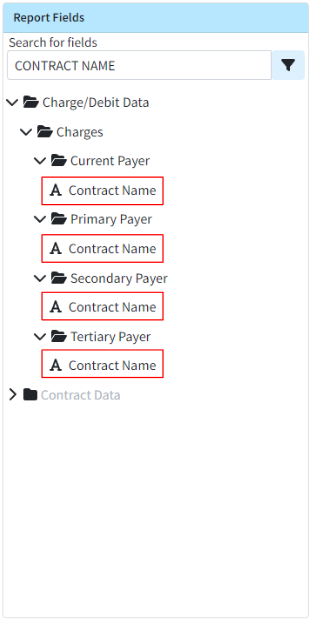
- New Report Fields For Patient Communication Preferences: We added the ability to include information about communication opt-ins in reports, enabling customers to conduct targeted outreach to patients to encourage them to opt-in. The following new communication preferences report fields have been added under Patient Data > Communications:
- Electronic Payment Plan Statements Communication Preference
- Electronic Statements Communication Preference
- Marketing Communications Preference
- Receipts Communication Preference
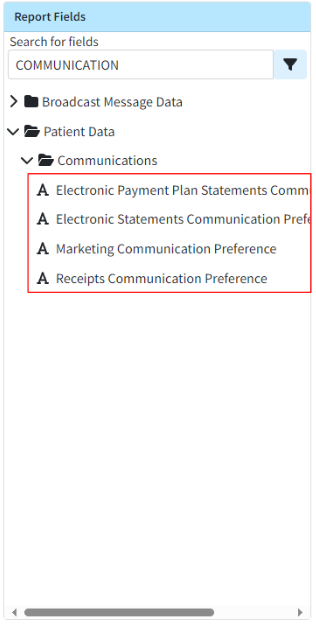
New Features and Updates
General
Patient
- New Statement Batch Print Search Options: We added the Default Provider and the Default Referring Provider as search (filter) options within Statement Batch Print, so only patients with the selected default referring or rendering providers are returned. This option will not affect the generated statement, which will continue to include all charges regardless of the rendering or referring provider on the claim.
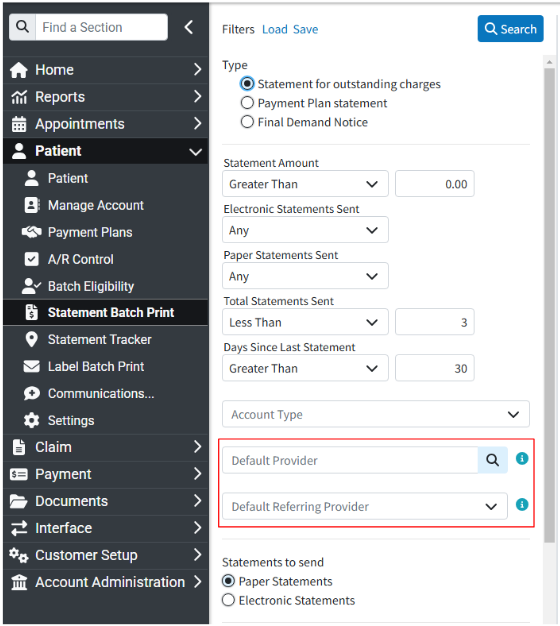
Payment
- Updated The Default ACCOUNT CREDIT & APPLY ACCOUNT CREDIT Memos: We updated the default account credit memo, created when an account credit is generated based on a payment or adjustment, to include more information about the credit. In this release, we also updated the APPLY ACCOUNT CREDIT memo line to include additional details (such as the source and check number) that will be visible in the Manage Account and Activity screens once the credit is applied.
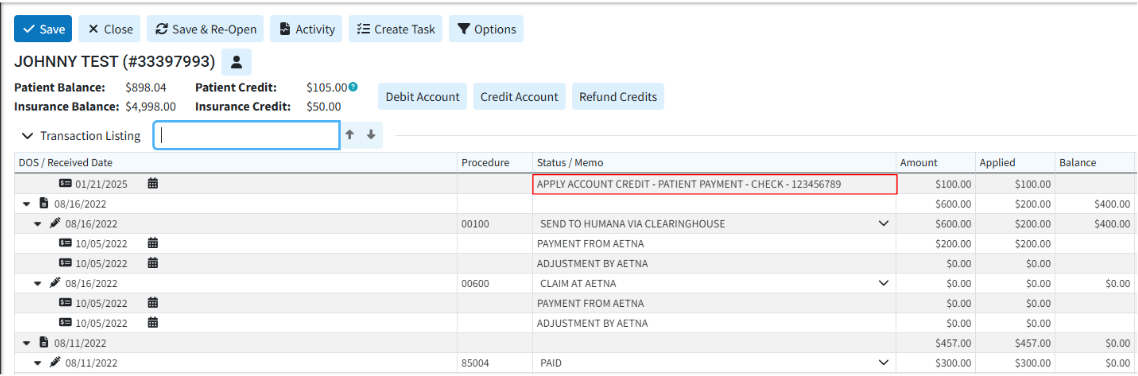
- New ERA Auto Post: Added a new ERA Auto-Post billing option that can be configured by Payer and pay priority (primary, secondary, etc.). Once enabled and configured, the Electronic Remittance Advice will automatically check for errors or warnings on most ERAs and, if the ERA is free of issues ("clean"), will automatically apply the payments with no interaction or review required.
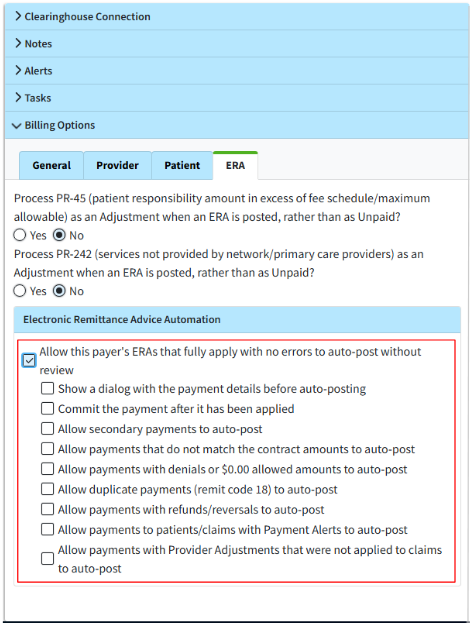 For more information on configuring this new ERA Automation billing option, please visit our ERA Billing Options Tab Help Article.
For more information on configuring this new ERA Automation billing option, please visit our ERA Billing Options Tab Help Article.
New Features and Updates
General
Appointments
- Added UI Improvements To The Scheduler's Eligibility & Forms Icons: We reduced the size of the Eligibility and Forms icons and allowed them to take up vertical space when available, enabling more appointment information to be visible on the scheduler. We also changed the color of the "intake forms sent but not filled out" icon from yellow to gray, distinguishing it from the "intake forms not sent" icon.
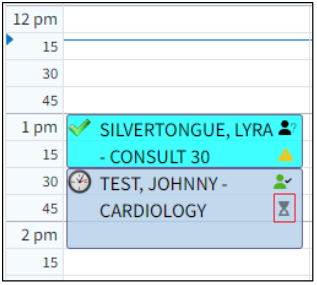
Patient
- Updated The Statement Tracker "Status" Column: Updated the Statement Trackers Status column to include the "user printed name." This allows users to see the print status, as well as the individual who printed the document, which improves the auditing process.
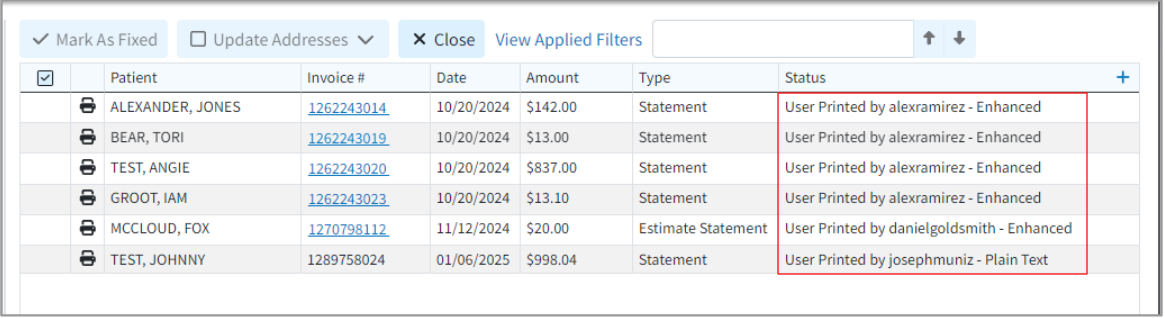
Claim
- New Enhanced Auditing (Show History) for Claims: CollaborateMD has been working on a new enhanced auditing project that provides offices with an easy and transparent way of auditing changes made in the application. We previously released our new Enhanced User Auditing feature in the Customer Setup and Patient sections of the application, allowing users to see a detailed list of changes made to specific records throughout the application.
In this release, we are expanding our Enhanced Auditing functionality to the Claim section enabling users to track modifications, changes, and updates made to claims within CMD for better auditing and accountability. With the new "Show History" feature, you can now determine which user changed specific Claim information in the software and when, by providing an auditing table with all updates or changes made to a record, including the user, date and time, and the item changed.
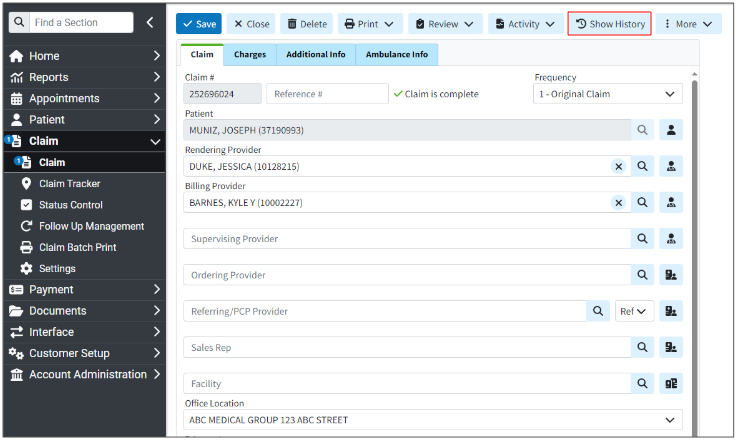
These new auditing records are also included in our existing User Audit Report, making it an even stronger tool for auditing multiple records simultaneously. The Show History capability has currently been deployed in the Customer Setup, Patient, and Claim sections, and we will be adding it to other sections of the application systematically.
For more information on using our new Add New Same/Similar Code List feature, please visit our Enhanced Auditing Help Articles.
- Status Control's "Current Payer" Column Update: Updated the Status Control results screen to show more details about which payer is displayed. The "Current / Primary Payer" column will now be "Current Payer," and will include the payer priority (primary, secondary, tertiary) in parentheses if the filtered charge status is a payer status.
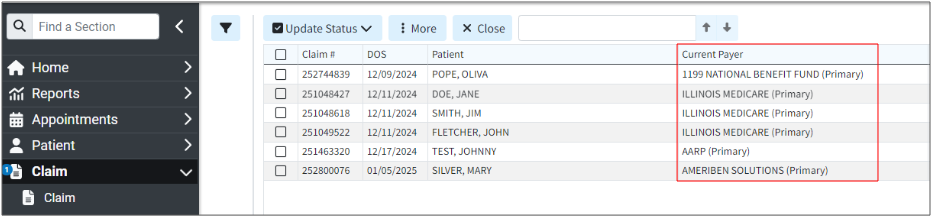
Customer Support
- New Signature Type Column Within Agreement Lookup: Added a new column, hidden by default, to the agreement lookup screen. This column will store and display the "Signature Type" (based on the Provider Action field received from ePS) and includes a new report field under Agreement Data. The possible actions for the "Signature Type" are:
- * Electronic Signature
- * Online Enrollment
- * Wet Signature
- * Other
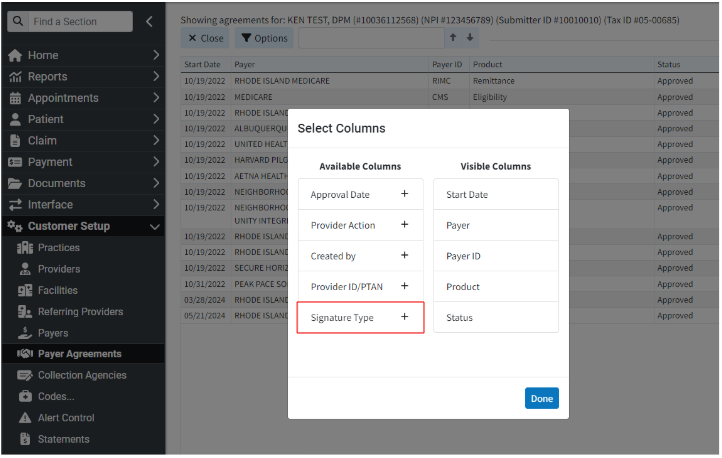
Payment Portal
- New UI Updates to The Payment Portal: Added some UI enhancements to the Payment Portal related to new colors and margins for better consistency and a better customer experience. We also updated the Payment Portals password requirements to now require at least 12 characters and disallow the reuse of any previous passwords.
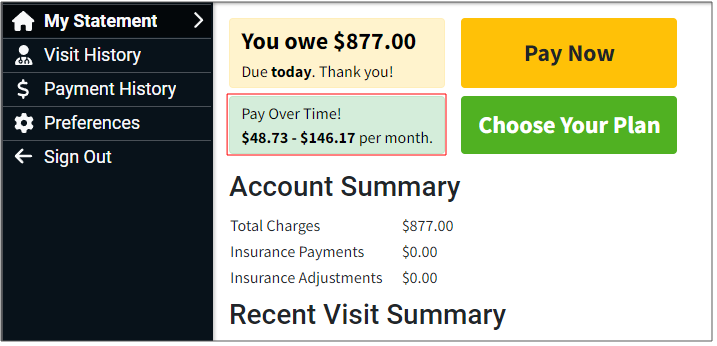
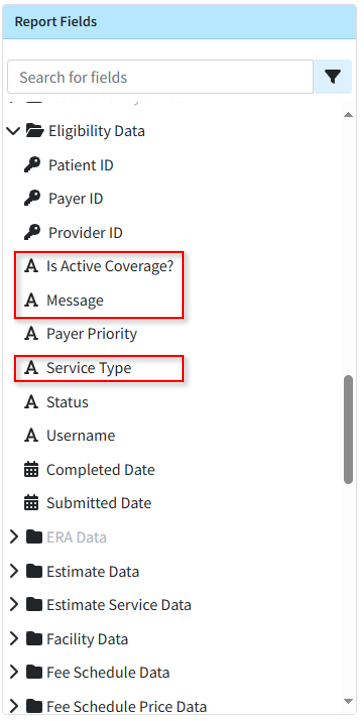
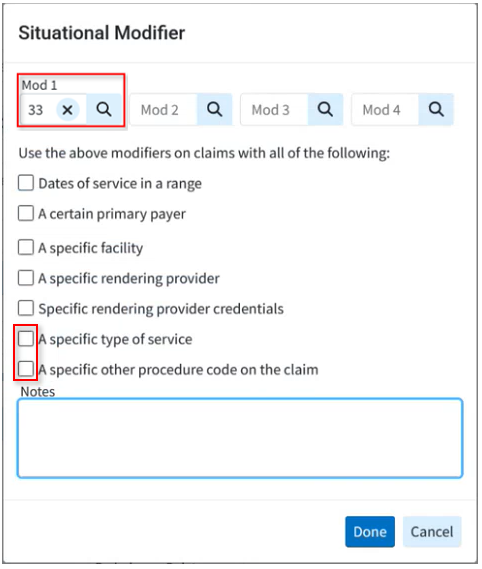
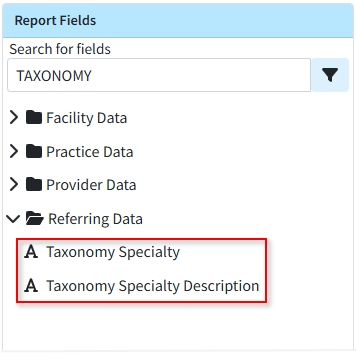
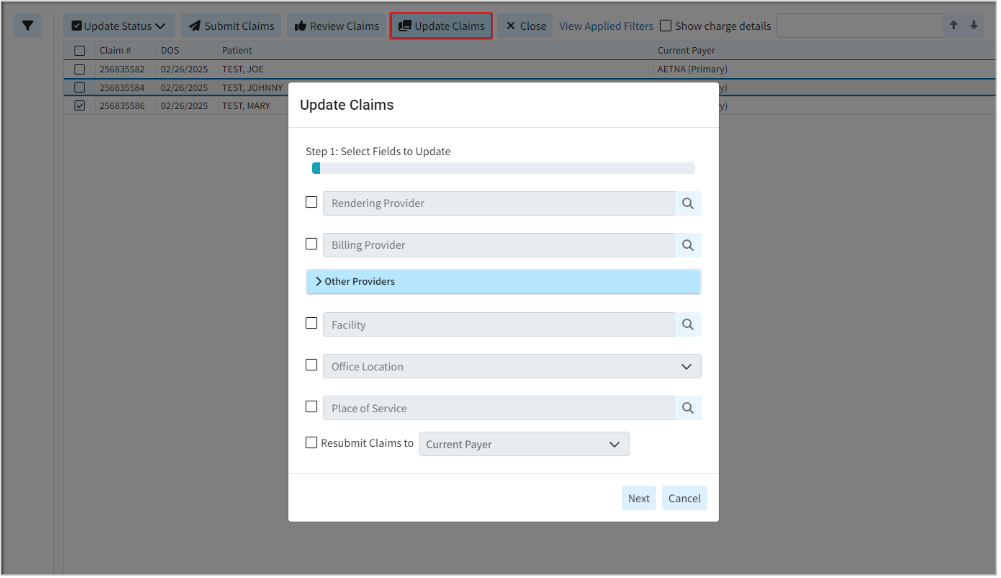
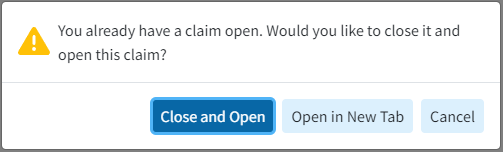
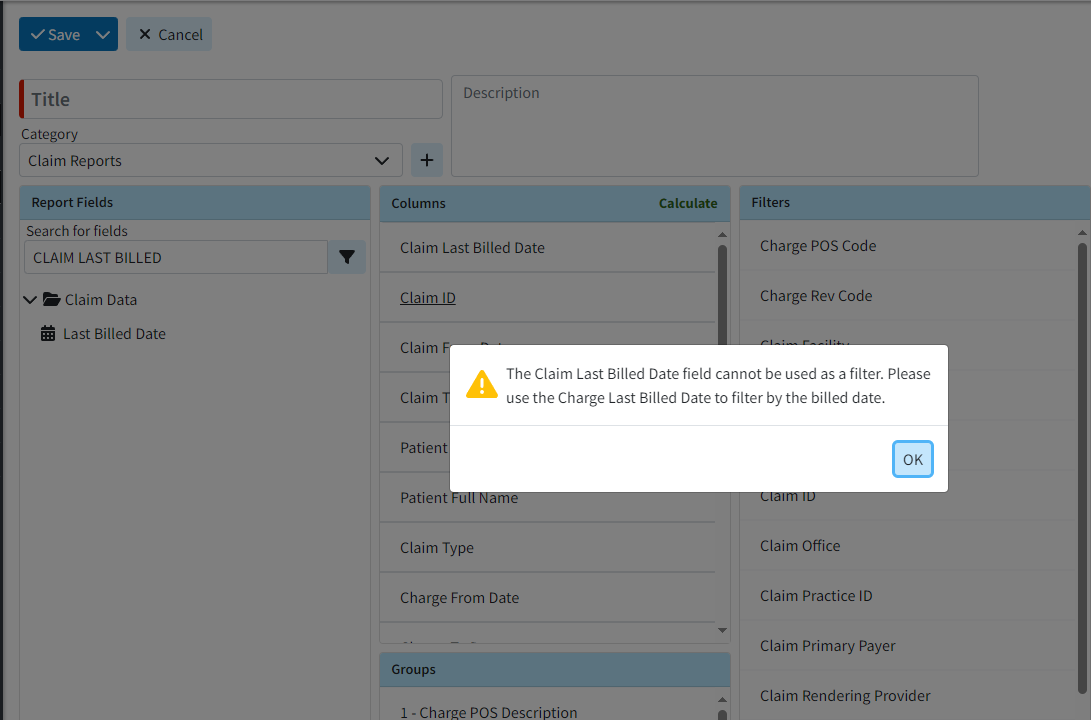
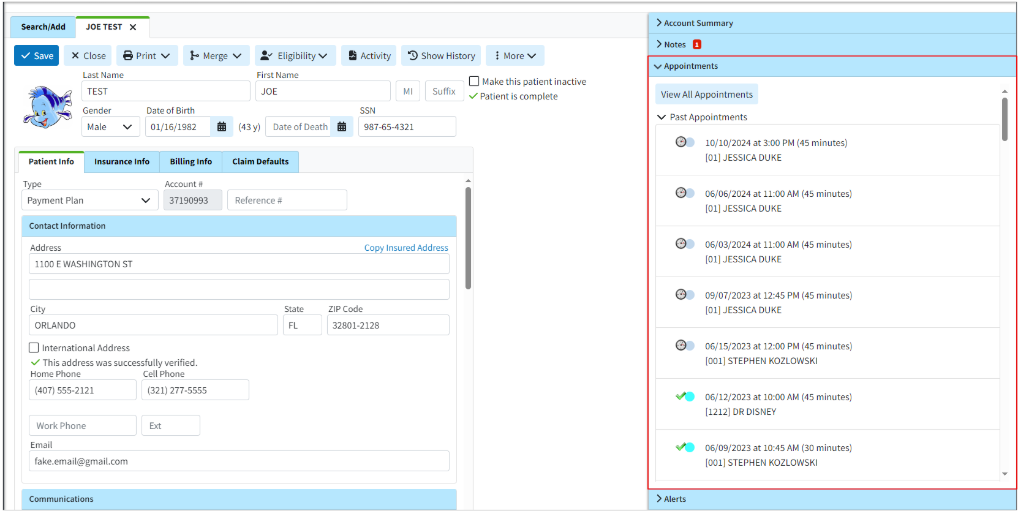
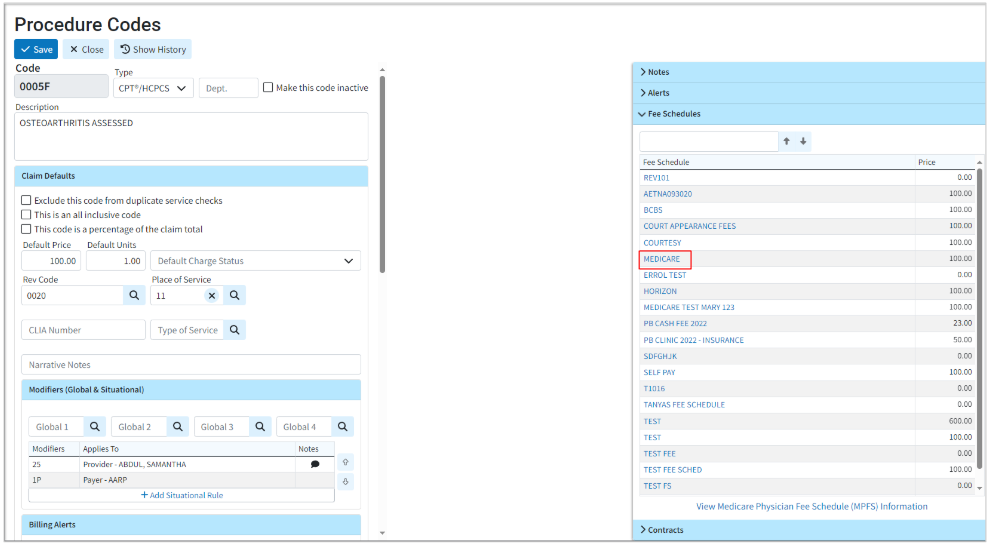
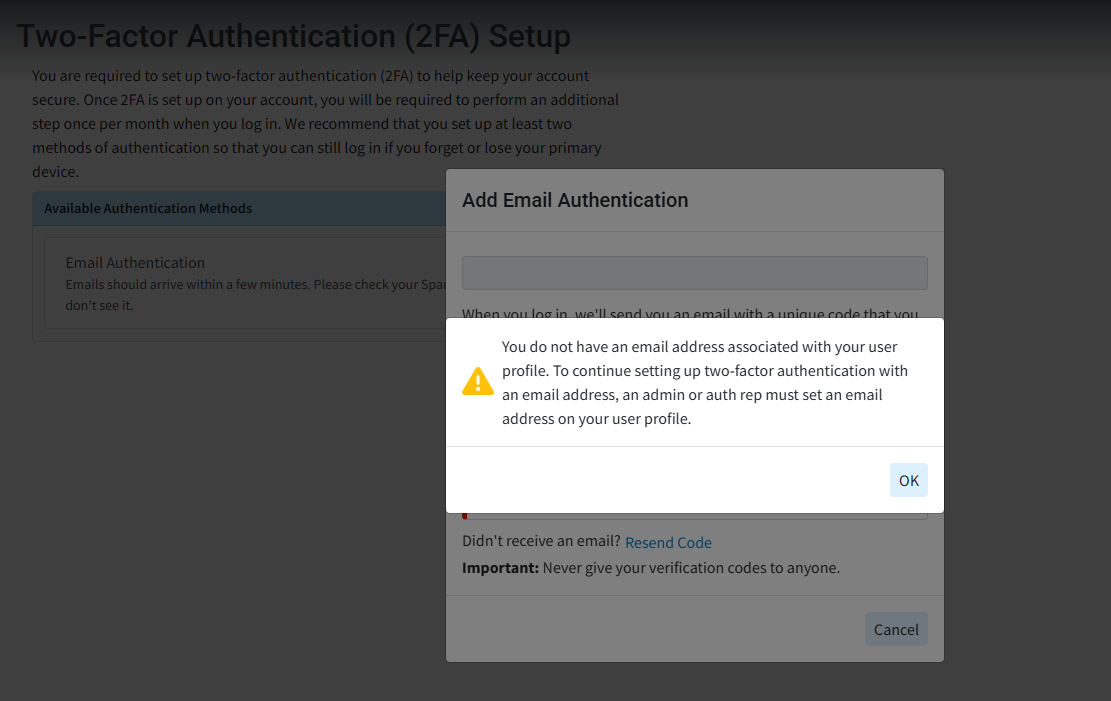
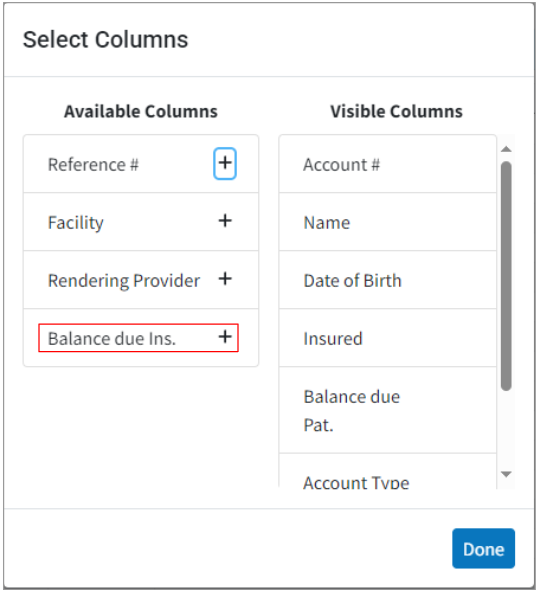
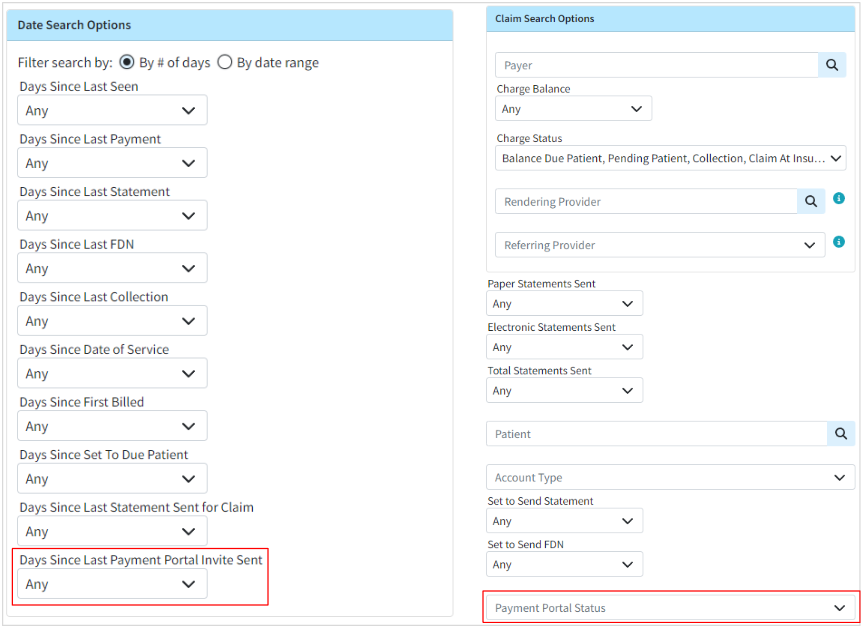 For more information on determining if patients have enrolled in the payment portal, please visit our
For more information on determining if patients have enrolled in the payment portal, please visit our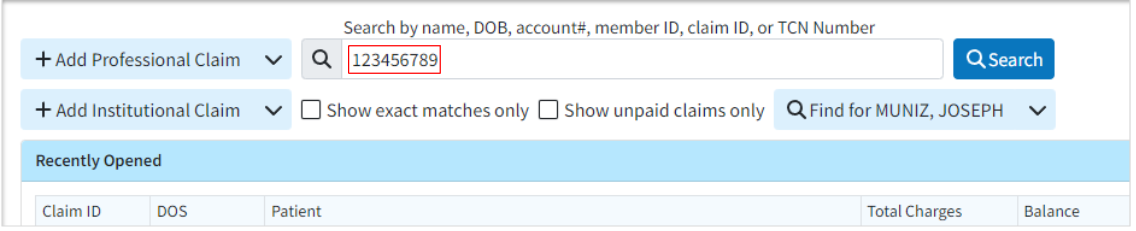
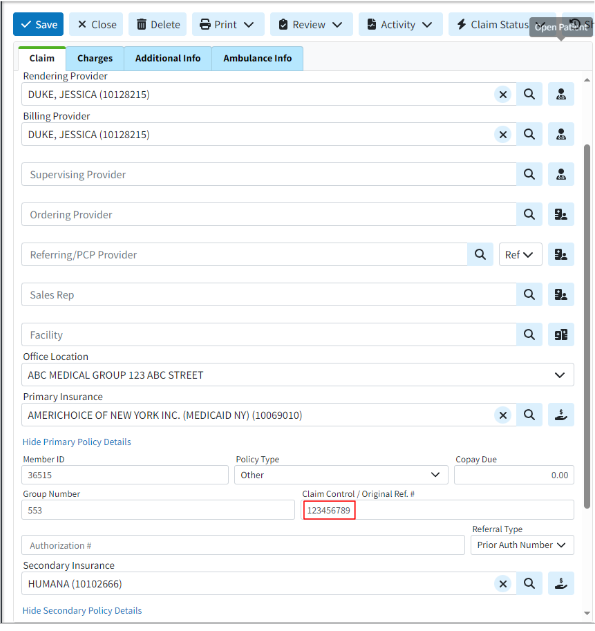
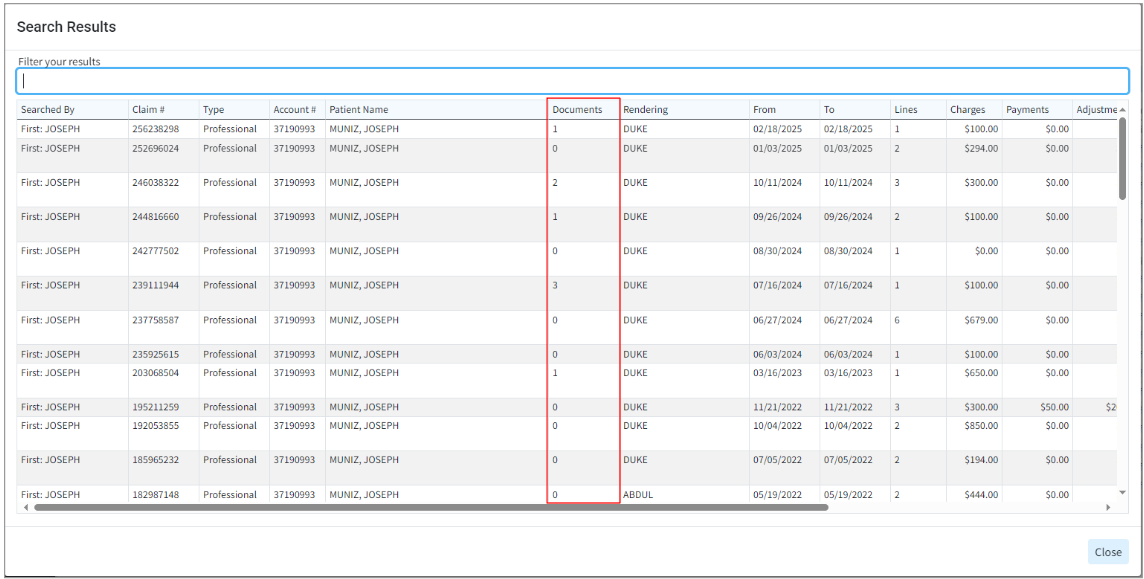
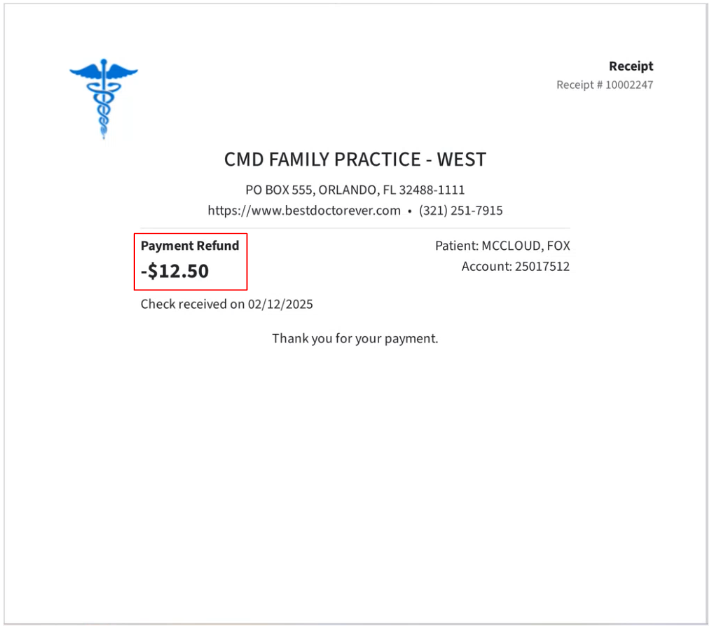
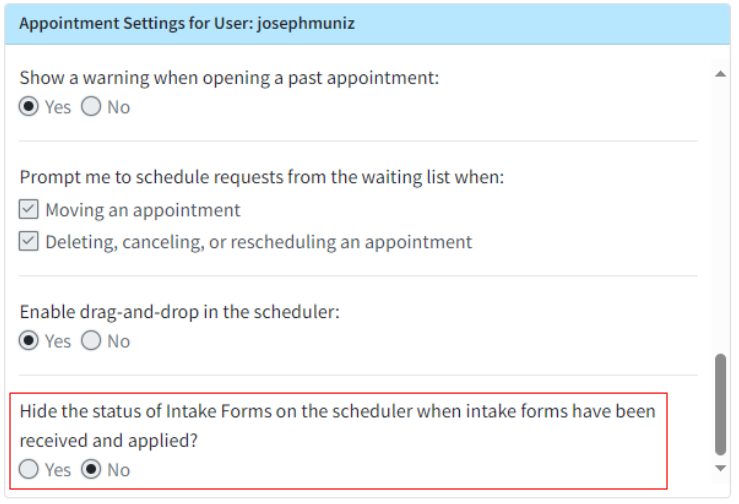
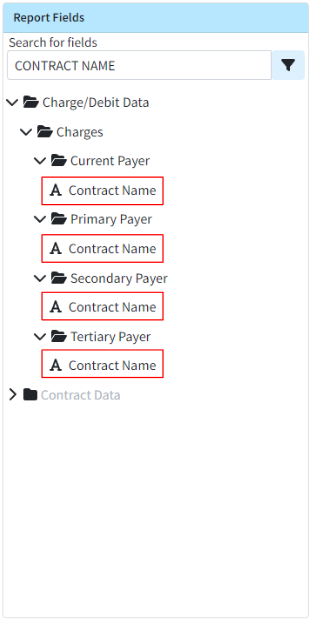
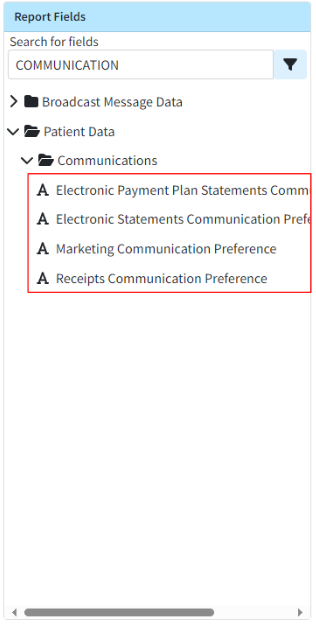
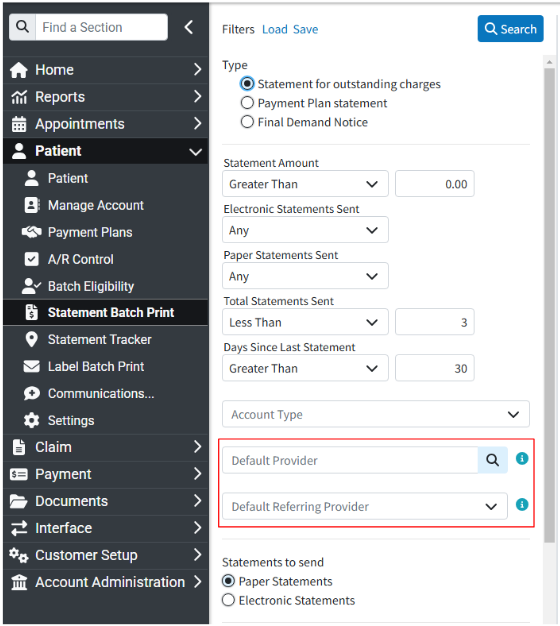
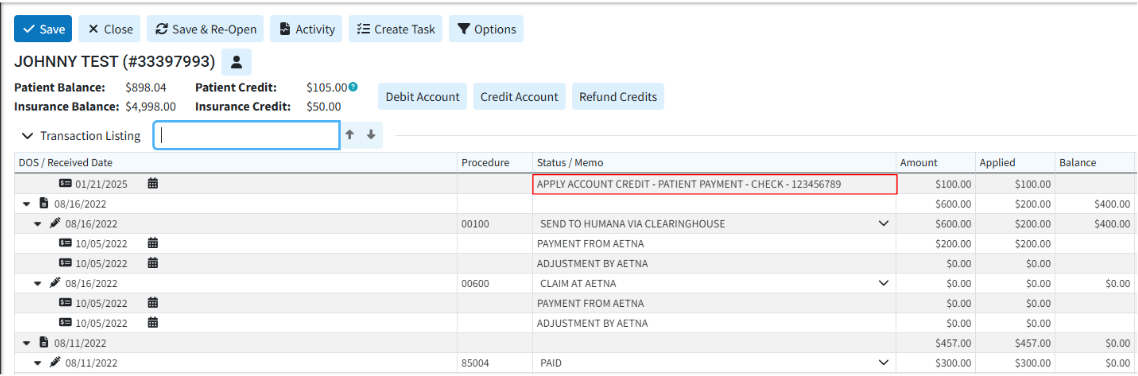
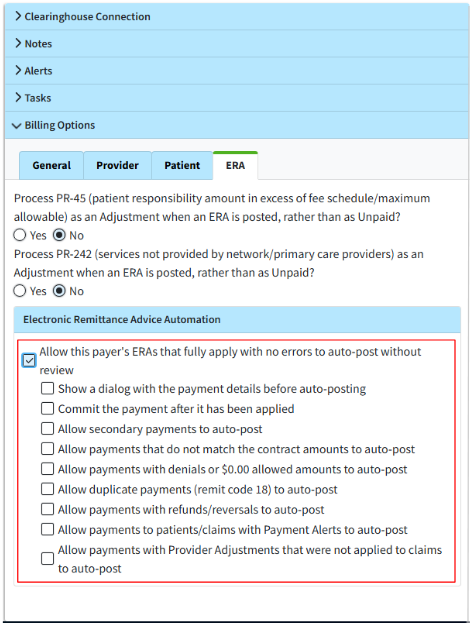 For more information on configuring this new ERA Automation billing option, please visit our
For more information on configuring this new ERA Automation billing option, please visit our