New Features and Updates
General
Reports
- Show Last Run Date and User for Custom Reports: We added the ability to store the Last Run Date and Last Run User on custom reports. This will provide users the ability to see the last time that a report was run, which is helpful for those customers who have a lot of custom reports.
When users right-click on a report from the Report Viewer and choose the "More Details" option, the resulting dialog will now additionally display the Last Run Date and the username associated with the report. Users will now see the following username/date & time data:
Created by user.name on date at time
Last updated by user.name on date at time
Last run by user.name on date at time
Patient
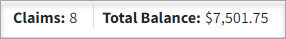
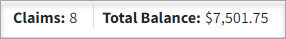
- New Search Bar in Manage Account: We added a search bar to the Manage Account screen. This will assist larger customers who see patients frequently in quickly locating a specific claim or payment by allowing them to easily search through their patients' information. The new "Find in Table" search field is available for the Transaction Listing, as well as the Account Credit Listing, and can be used to search by dates, procedure, status, amounts, etc.
Visit our Find Payment Transactions Help Article for more information.
Claim
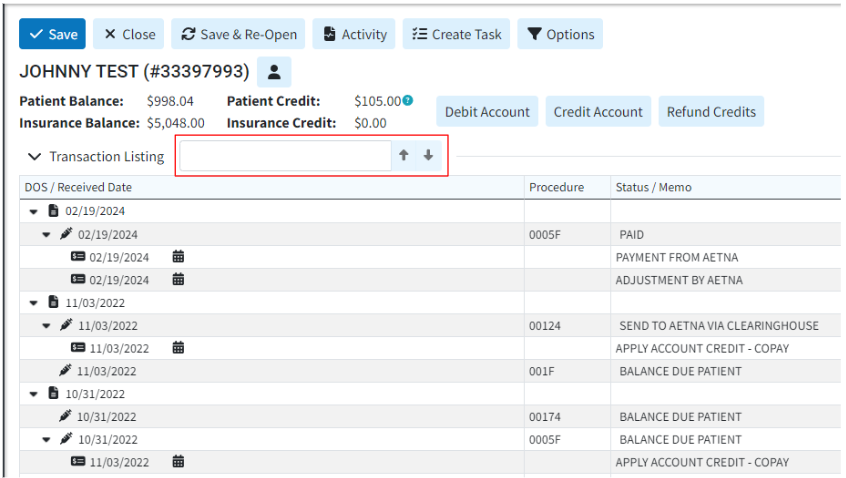
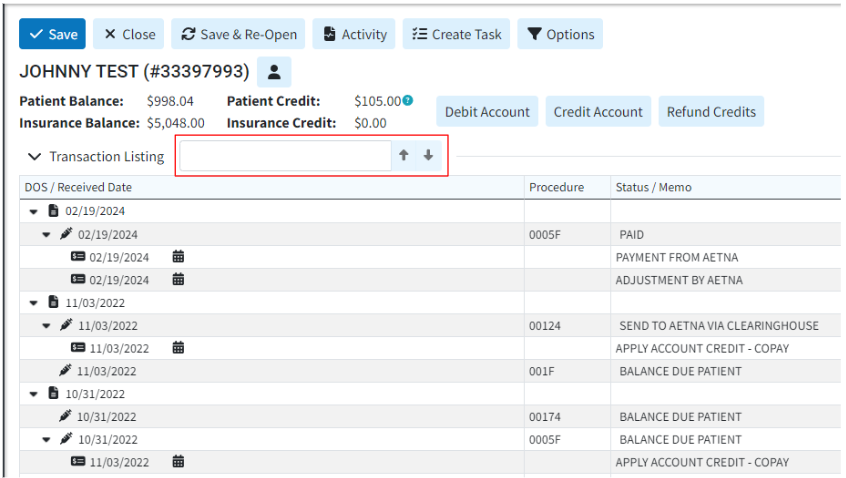
- Removed the "Relative" option when viewing Notes in the Patient section.: Removed the word "Relative" when viewing notes in the Patient section since the option has no effect. We also changed the “Relative Notes” wording from other sections as follows:
- In the Claim section, it now reads “Notes for This Claim”
- In the Payment section, it now reads “Notes for This Payment”
- In the Appointment section, it now reads “Notes for This Appointment”.
Payment
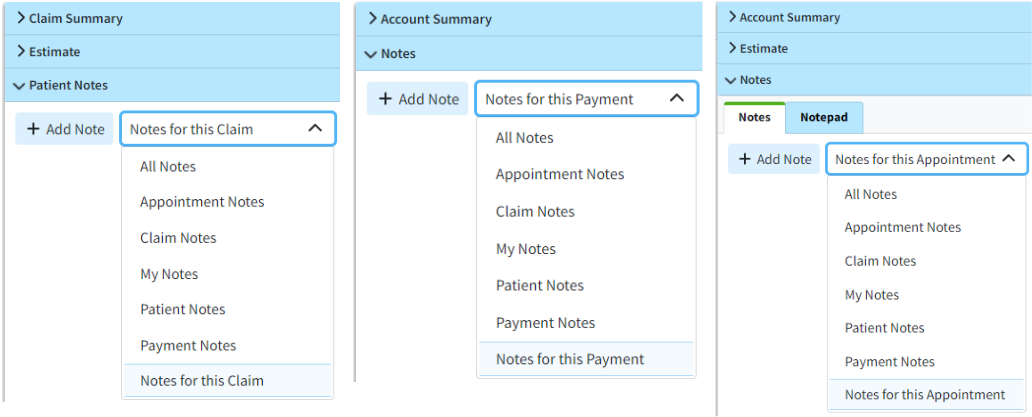
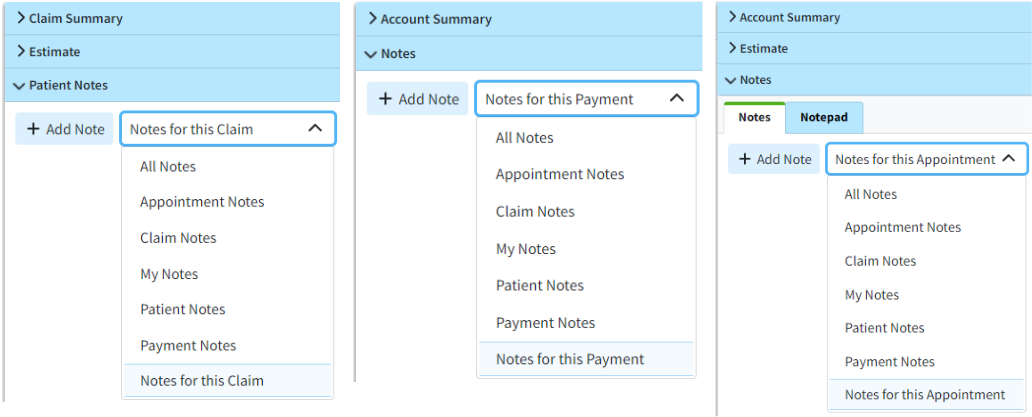
- New Optional Column to Display Rev Code on Patient Payments: We added a new optional column hidden by default for the Rev Code on Patient Payments. This column can be added using the visual indicator for the Table Header Features (+ symbol), or the right-click option to select columns.
Customer Setup
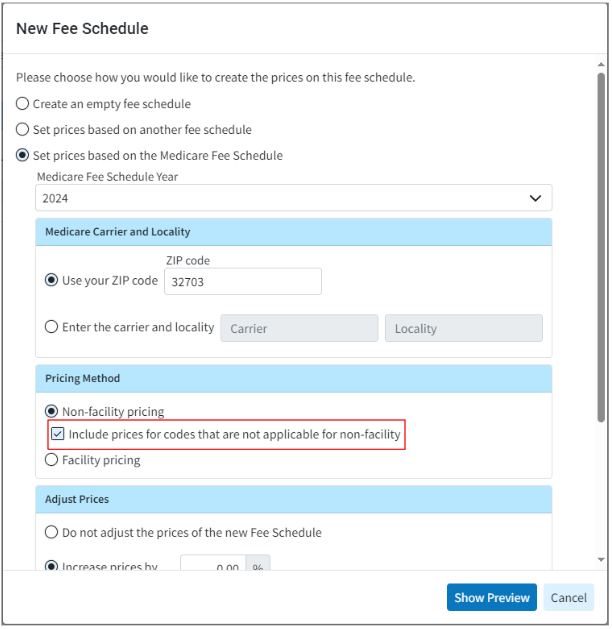
- Allow Including Codes Not Applicable for Non-Facility Pricing For Medicare Fee Schedule: We previously corrected our system to ensure it does not return a price in the Medicare Fee Schedule's non-facility pricing for codes that are not applicable. However, some users still want to use those prices when building their fee schedules, as they base their fees on the Medicare fee schedule but do not necessarily submit all claims to Medicare. In this release, we added a new checkbox option when selecting Non-facility Pricing while creating a Fee Schedule or Contract using the Medicare Fee Schedule. When checked, the option to “Include prices for codes that are not applicable for non-facility” will return the price even if the code is marked as “not applicable” for non-facility pricing in the Medicare Fee Schedule.
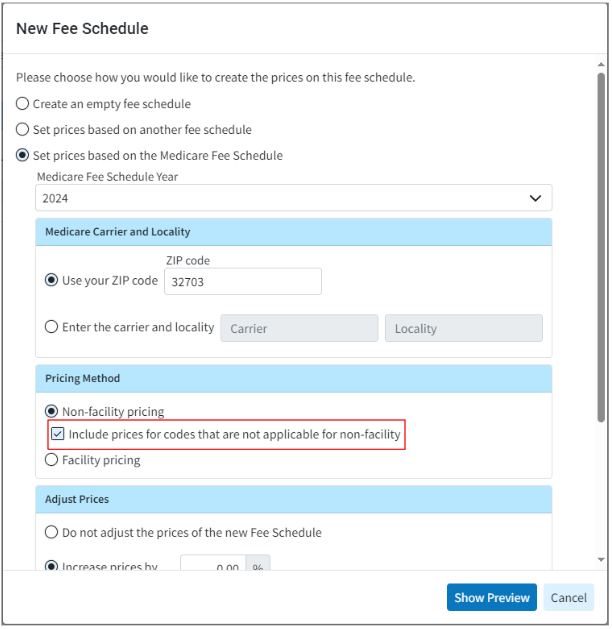
For more information on setting prices based on setting the pricing method on a fee schedule, visit our Add a Fee Schedule Help Article.
New Features and Updates
General
Reports
- New "Open Negotiation Form" Report Fields: We recently added two new fields to the Claim section under Follow Up Management → Open Negotiations to track the Open Negotiations Period End Date, which is 30 business days after the letter has been submitted, and the Federal IDR Initiation Deadline Date, which is 4 business days after the end of the Open Negotiations Period. In this release, we added two new report fields associated with these Open Negotiation deadlines. These 2 new fields are available under Claim Data → Follow Up Activity are:
- Federal IDR Initiation Deadline Date
- Open Negotiations Period End Date

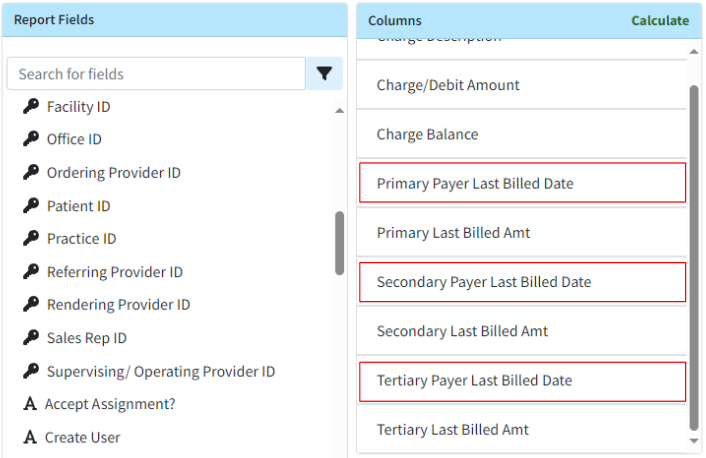
- New "Last Bill Date" Report Fields: We added 3 new report fields for the last billed date based on the payer priority. These new fields are available under:
- Claim Data → Primary Payer → Last Bill Date: This field will show the latest Activity Entered Date for the claim’s current Primary Payer.
- Claim Data → Secondary Payer → Last Bill Date: This field will show the latest Activity Entered Date for the claim’s current Secondary Payer.
- Claim Data → Tertiary Payer → Last Bill Date: This field will show the latest Activity Entered Date for the claim’s current Tertiary Payer.
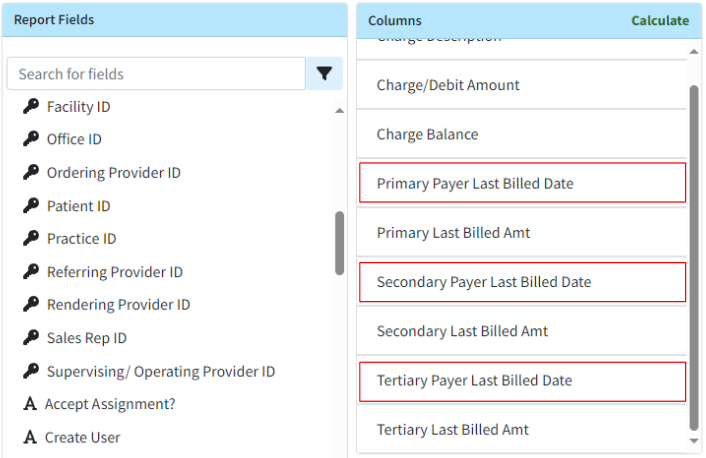
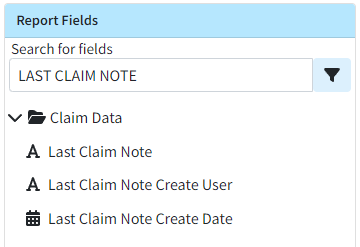
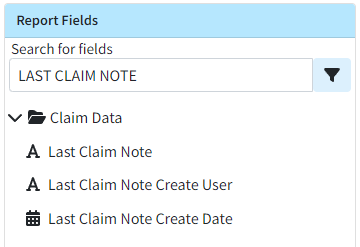
- Last Claim Note Report Fields Now Available: Currently, users can add fields related to the most recent Claim Follow Up Note to a report by using the “Last Public Claim Follow-Up Note” fields. We also have similar fields for the “Last Claim Note,” but these fields were not visible. In this release, we have updated the following fields to make them no longer hidden.
- Claim Data → Last Claim Note
- Claim Data → Last Claim Note Create User
- Claim Data → Last Claim Note Create Date
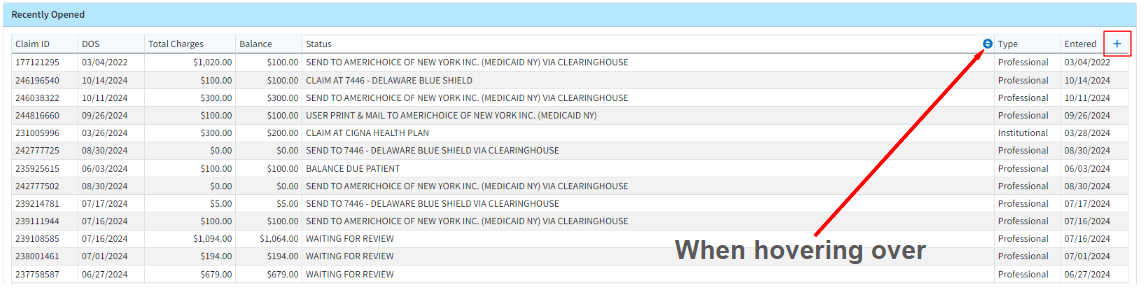
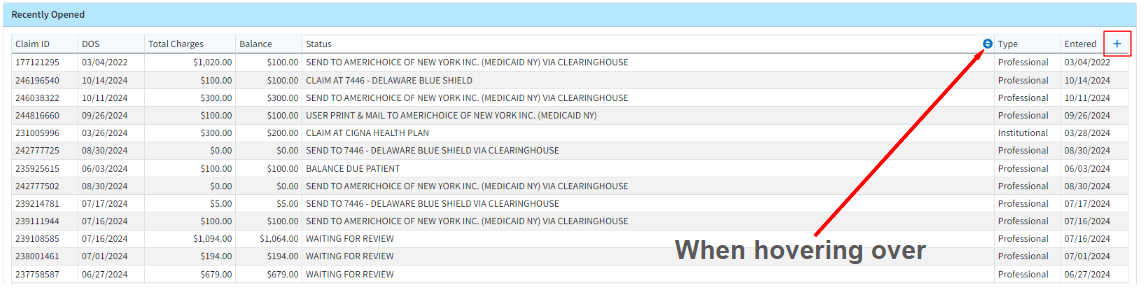
Claim
- New Visual Indicator of Table Header Options: We have added a visual indicator for the Table Header Features, which include Sorting, Rearranging columns, and Hiding or showing columns. These features were previously accessible through right-click actions, but we have now provided a more visual representation of these functionalities. Clicking the + symbol on the rightmost table header will open the show/hide columns dialog (only for tables that support adding or removing columns). When hovering over a column header, a blue up/down arrow appears on the table header. Clicking this arrow will then provide the user with header actions, such as the ability to sort the column, rearrange the column order, or hide the column.
Customer Setup
- Allow Setting The Cost Of Goods And Services: Some users offer services with an associated cost and/or pay their providers based on the profit from these services provided. To support this workflow, we added the ability to track the Cost of Goods and Services (COGS) within the application.
-
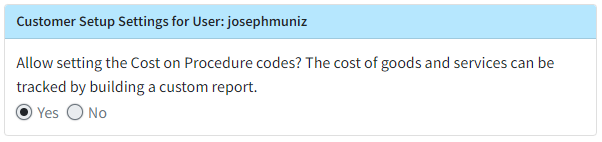
We added a new Settings section under Customer Setup containing a User-based setting: "Allow setting the Cost on Procedure codes? The cost of goods and services can be tracked by building a custom report."
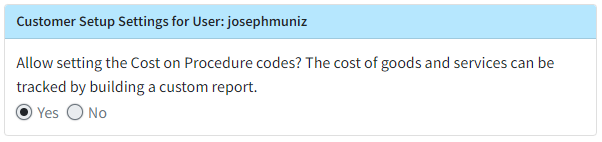
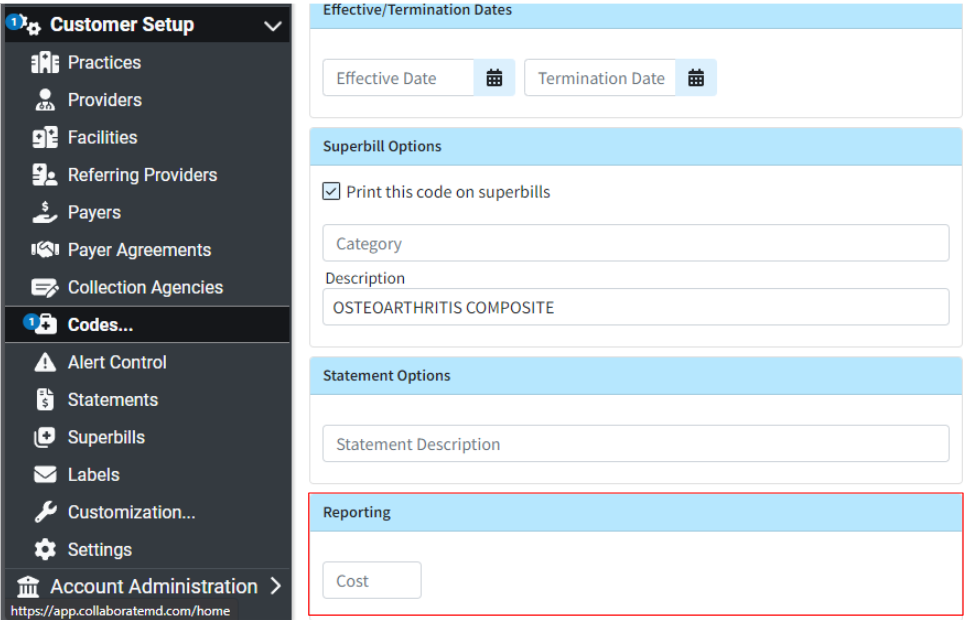
- If set to Yes, a "Reporting" option will be added to Procedure Codes allowing the user to add a cost to the code.
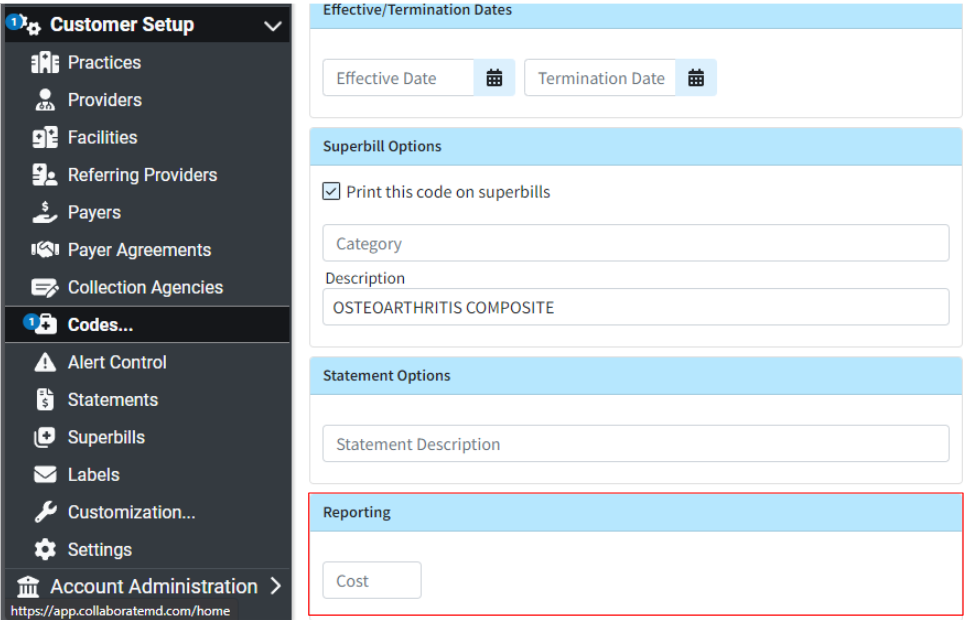
- If set to Yes, a "Reporting" option will be added to Procedure Codes allowing the user to add a cost to the code.
-
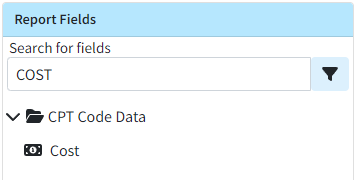
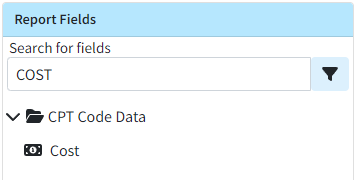
We also added a new report field under CPT Data → Cost, which, when added to a report, will return the amount entered for that procedure code.
-
For more information on our new setting, visit our Customer Setup Settings For User Help Article.
New Features and Updates
General
Services
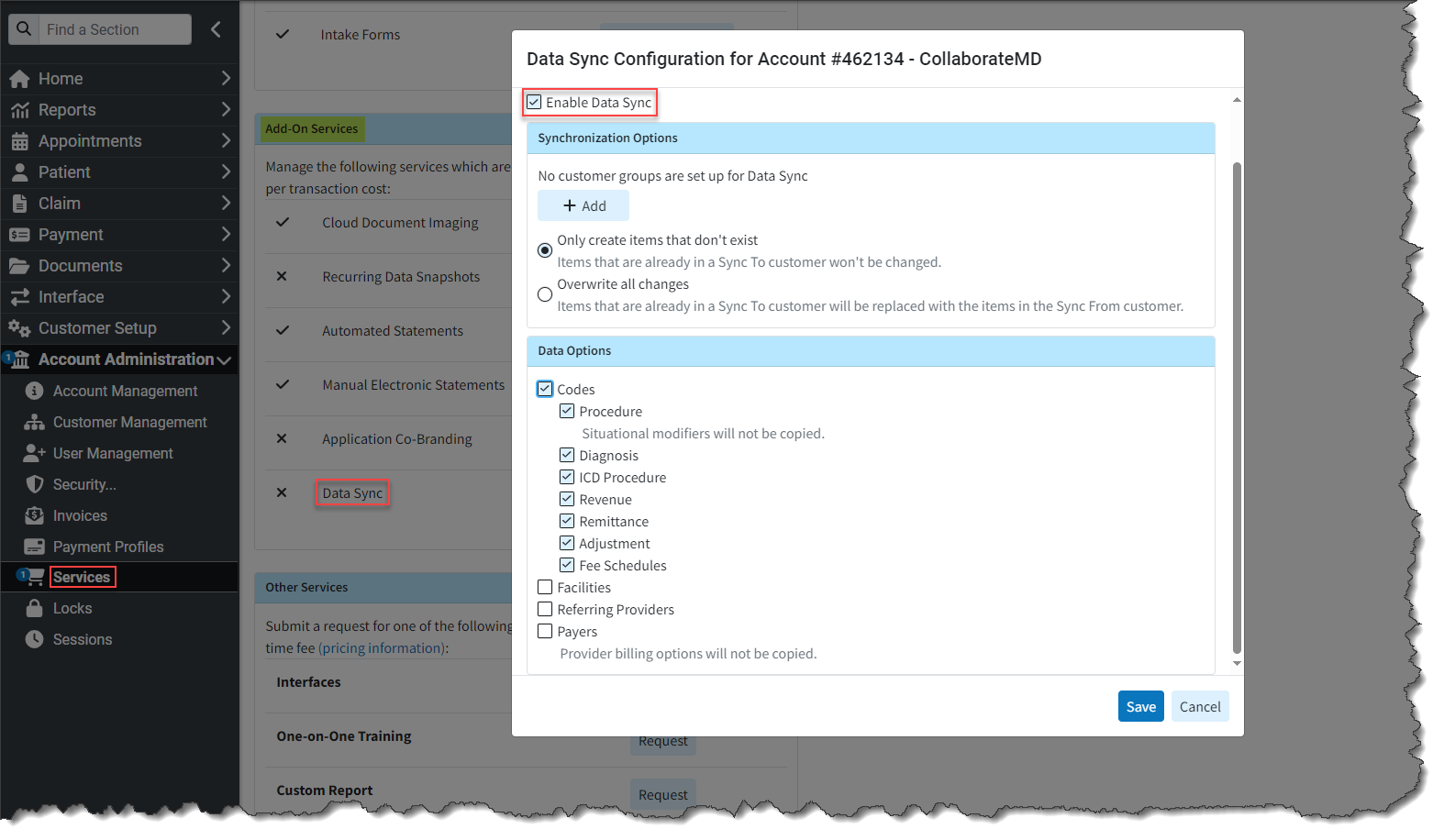
- New Data Sync Service: Many of CollaborateMD's customers are healthcare practices or billing service providers that operate across multiple states and have separate customers under their main accounts. This structure enables them to maintain distinct data for patients, claims, and payments for each customer. However, this setup also requires users to independently input setup data such as referring providers, facilities, various codes (procedure, fee schedules, diagnosis, remittance, revenue, etc.), and payers for each customer, resulting in significant setup work. Some of this work could previously be mitigated by requesting a manual, one-time data copy.
To convert this manual process into a completely automated solution, we created our Data Sync feature. Data Sync is a fully automated process that enables clients to automatically synchronize their data with multiple customers whenever an update is made. This feature will replace the Data Copy function but at a reduced cost for customers. By automating the process, it will enhance productivity within CMD and save time by eliminating the previous manual work required across multiple CMD departments when completing a Data Copy.
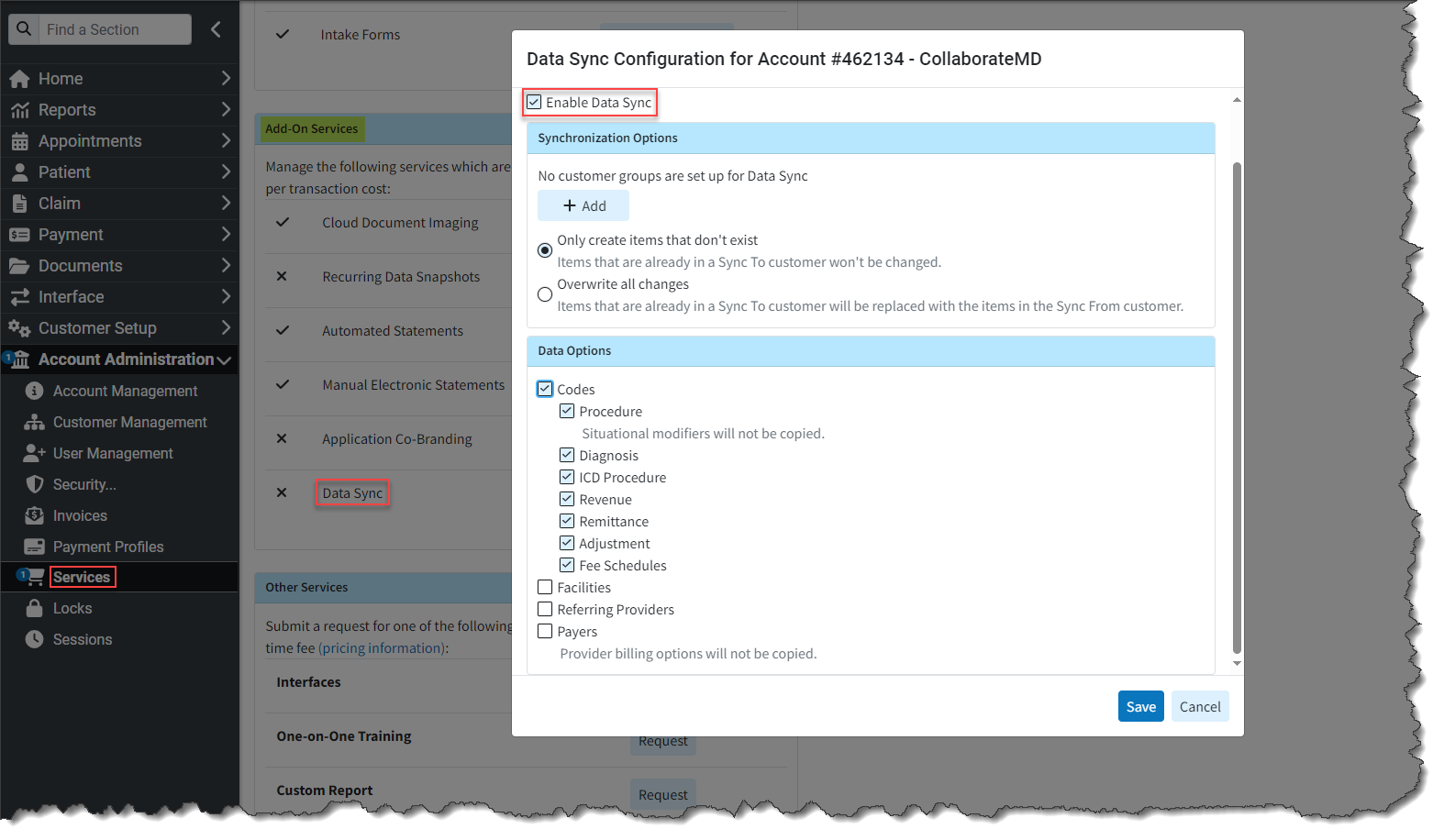
For more information on enabling or using our new Data Sync feature, please visit our Manage Data Sync Help Articles.
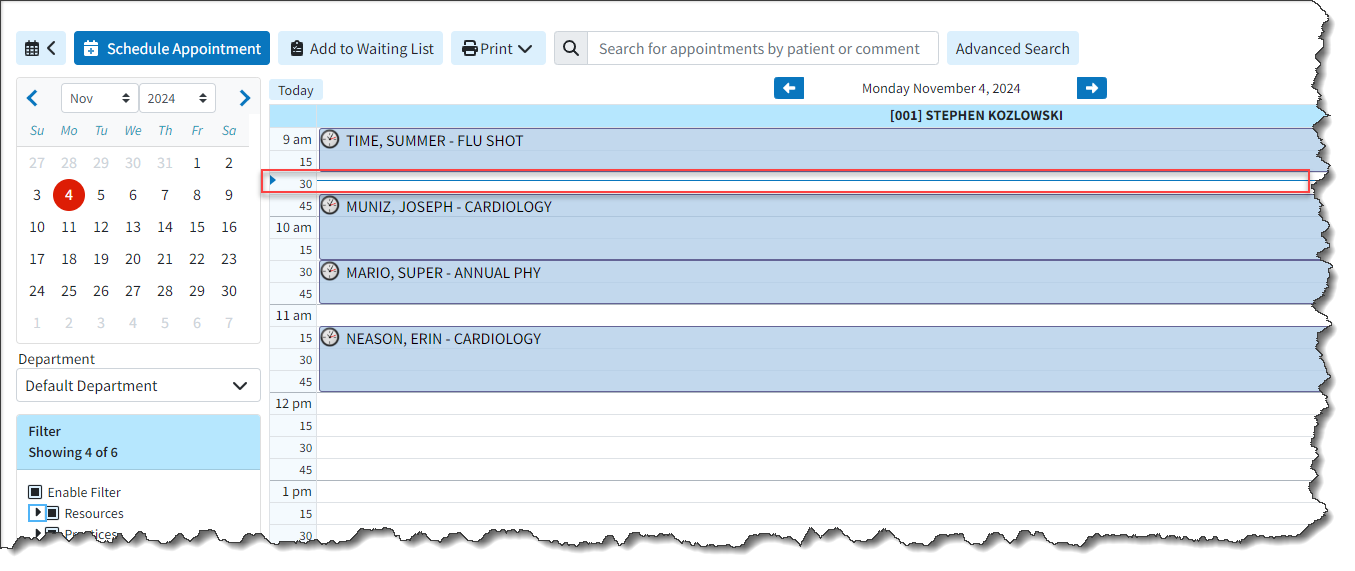
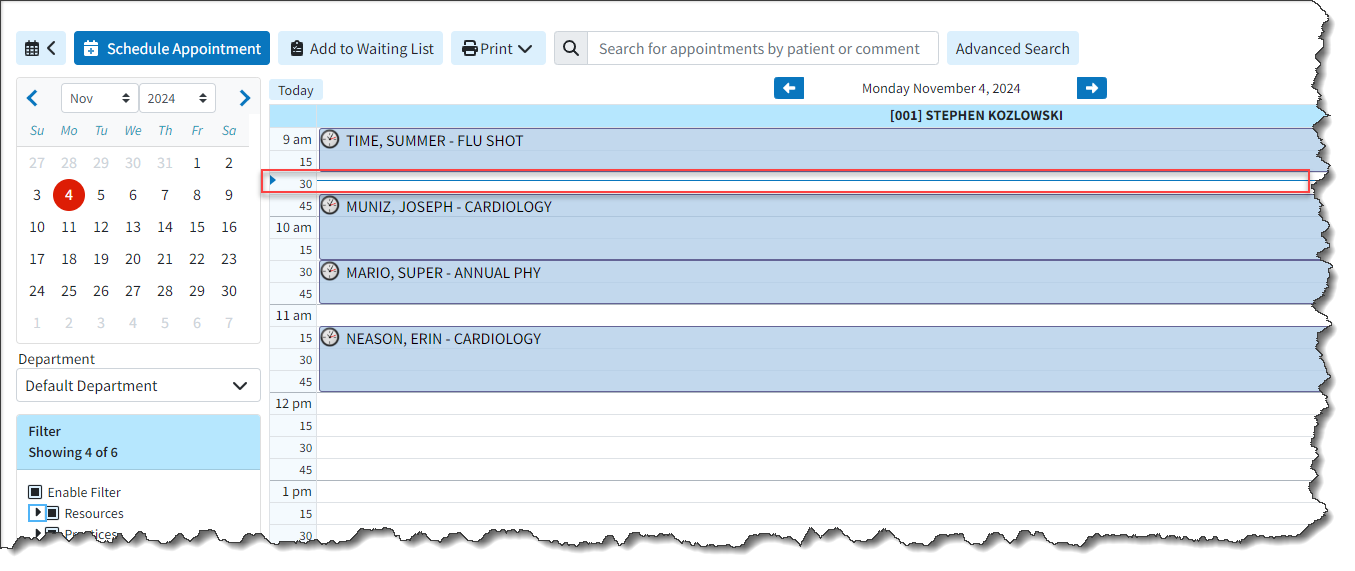
Appointments
- New Scheduler Visual Time Indicator: We added a new visual indicator (represented by a blue line) to mark the current time of day within the Scheduler. This feature enables the user to readily identify the current appointment or time slot within the scheduler. Additionally, we modified the process of closing an appointment in the Scheduler to automatically scroll back to the previous position (time) within the calendar.
Claim
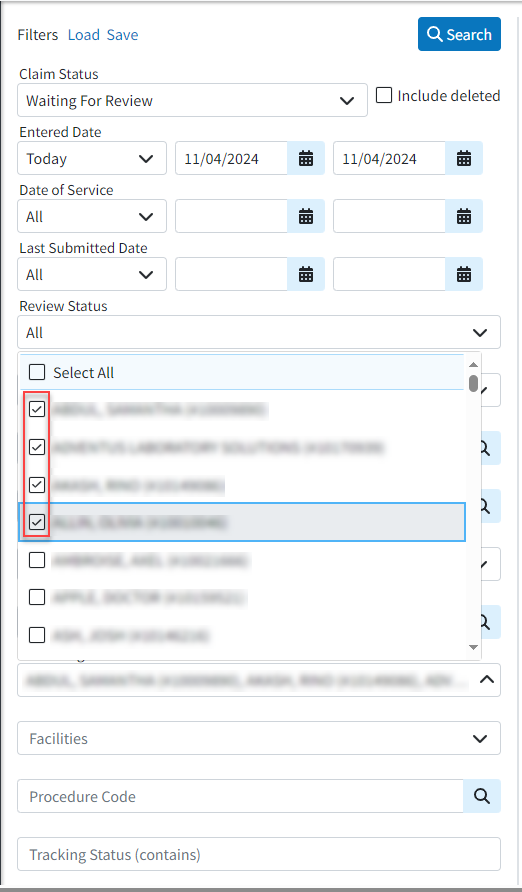
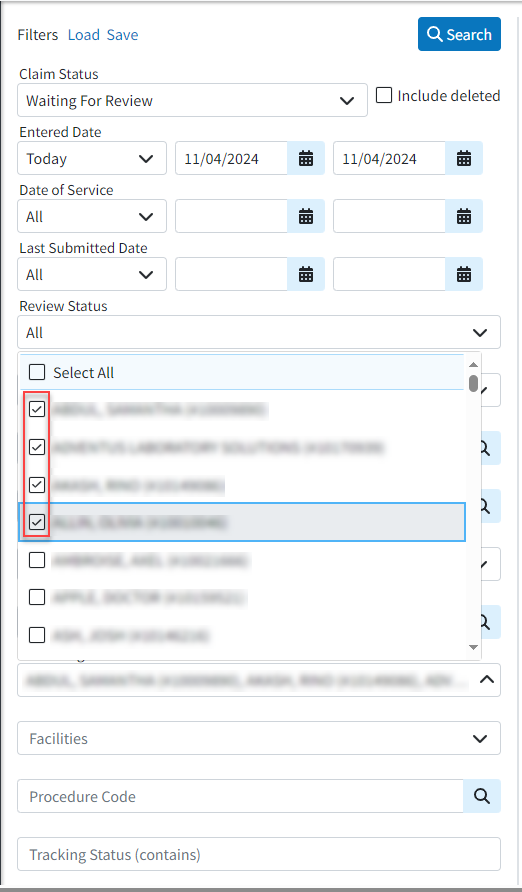
- Multi Select Status Control Filter for Rendering Provider & Facilities: We updated the Status Control filters to enable searching by multiple rendering providers and facilities (using checkboxes). This change mirrors the functionality we have previously implemented in other sections, such as the claim tracker.
- Update to Prevent Users Without the Claim Delete Permission From Deleting Previously Billed Charge Lines: We added an update in all areas where charges can be deleted (the Claim section and Manage Account) to prevent users without the "Claim Delete" permission from deleting charge lines that have already been billed. This means that only users with Access, Modify, & Delete permissions can access, modify, and delete a claim or charge.
Customer Setup
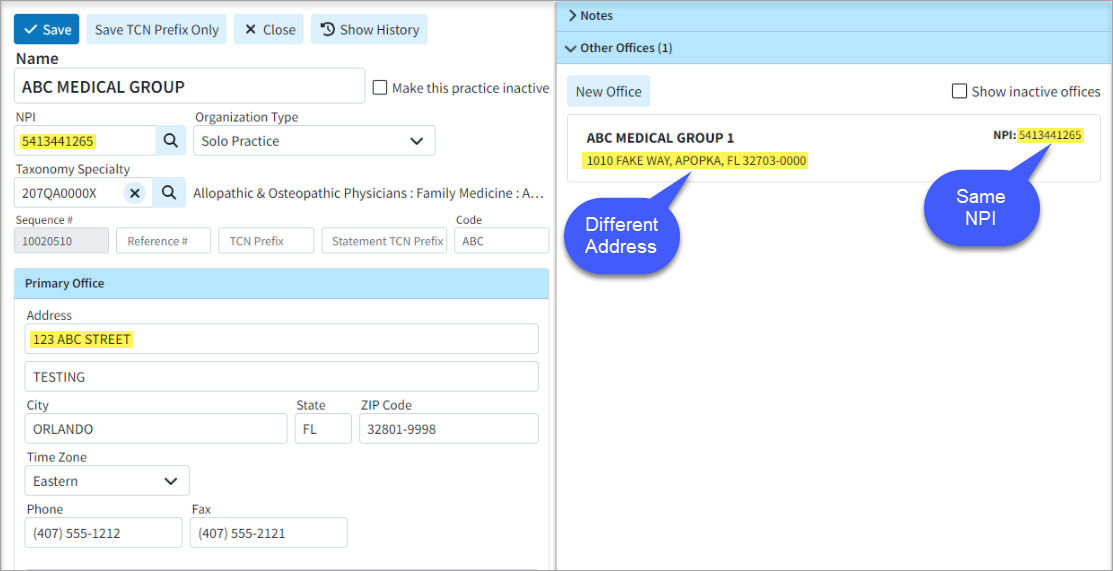
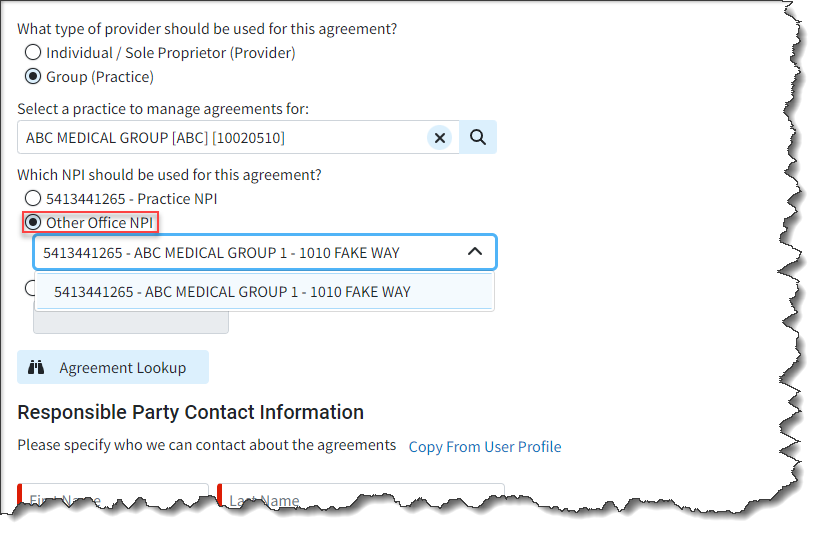
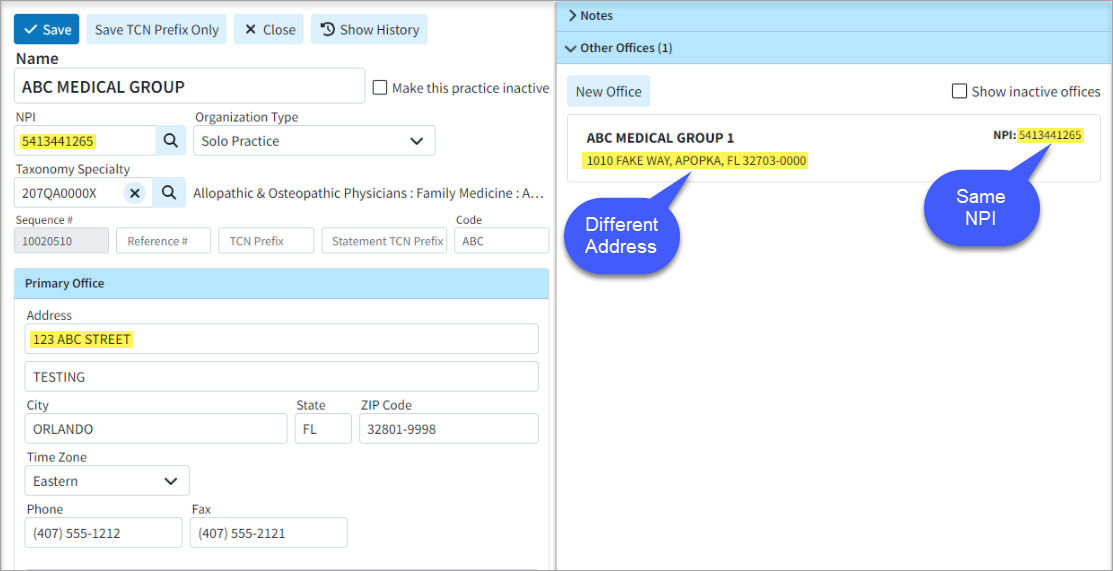
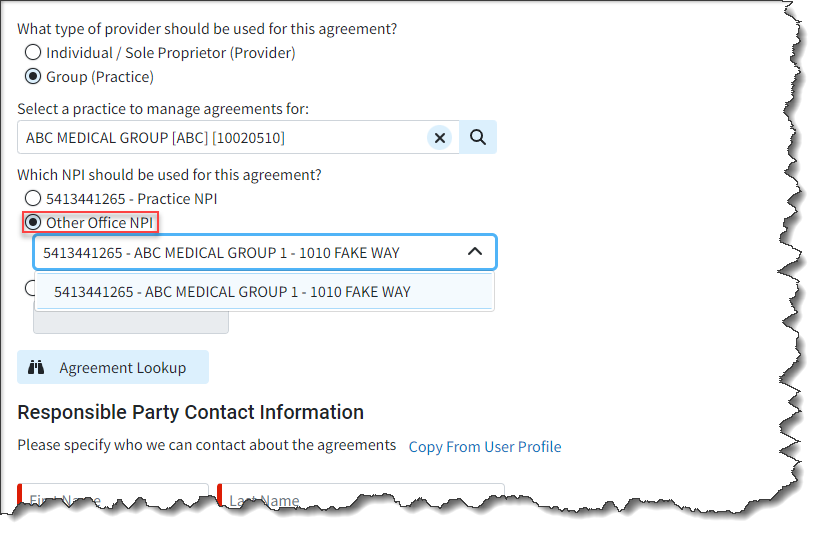
- Updated the Payer Agreement Option for "Other Office NPI" to Include Same NPI/Different Address Scenarios: We added the ability to allow selecting different office addresses for Payer Agreements even if the NPI is the same. For Practices with multiple offices, this new option gives you the ability to use the "Other Office NPI" option as long as any of the other office(s) has a different NPI or Address than the practice. This will help customers in scenarios where payers have different addresses on file for the same NPI.
New Features and Updates
General
Customer Setup
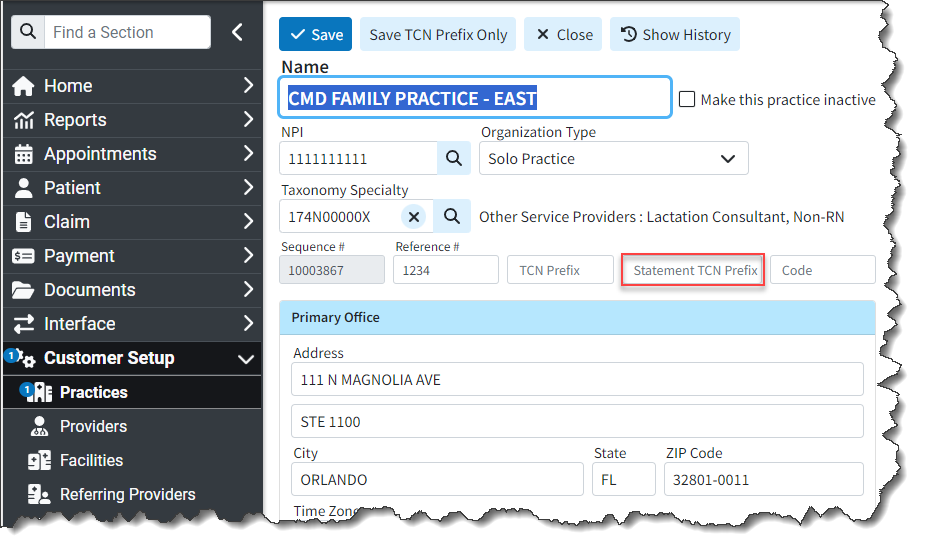
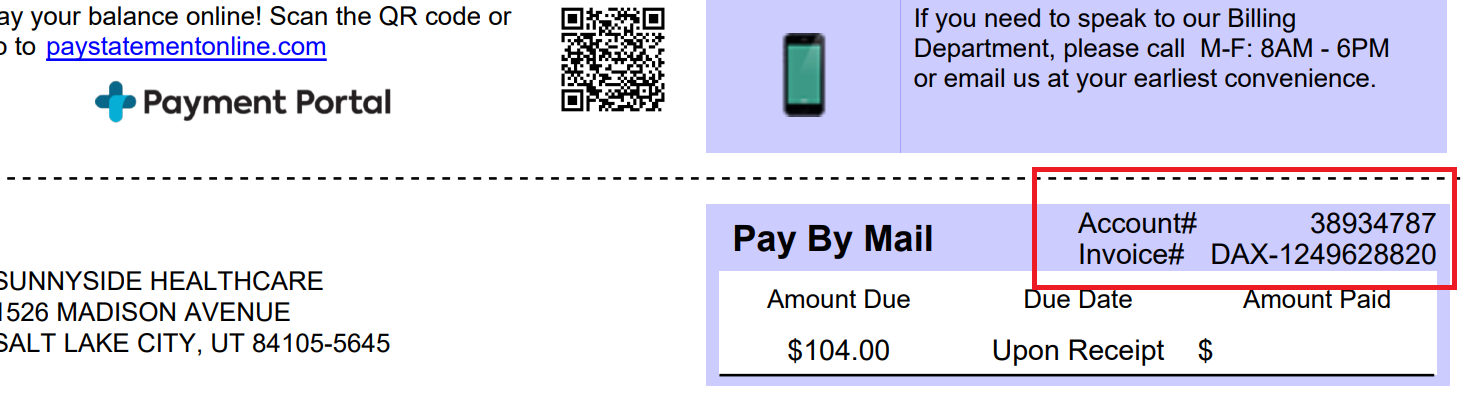
- New TCN Prefix for Statements: We added a new Statement TCN Prefix within the Practice section, allowing customers to display a custom identifier on their statements. This will help them identify which system produced the statement and where to post it. When added, the statement's invoice number will show the TCN prefix, followed by a dash and the TCN (for automated and enhanced statements).
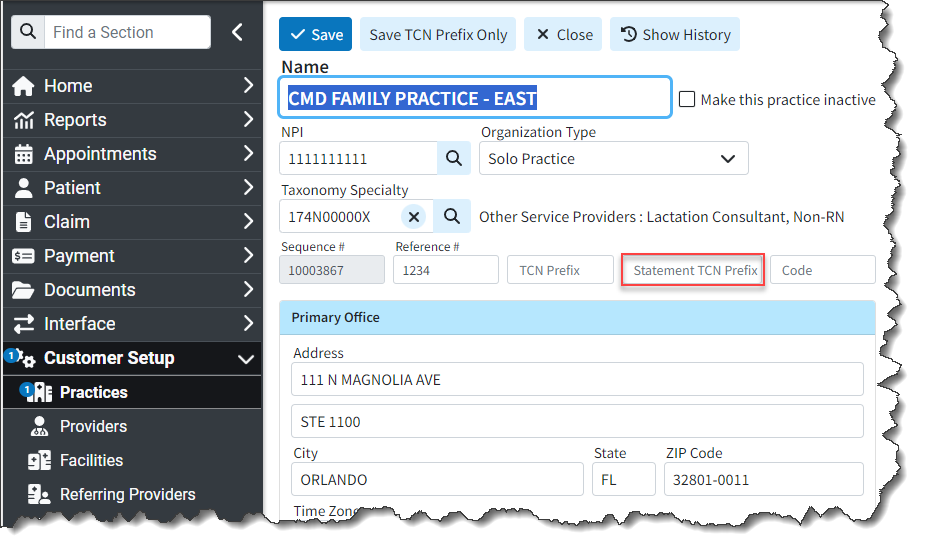
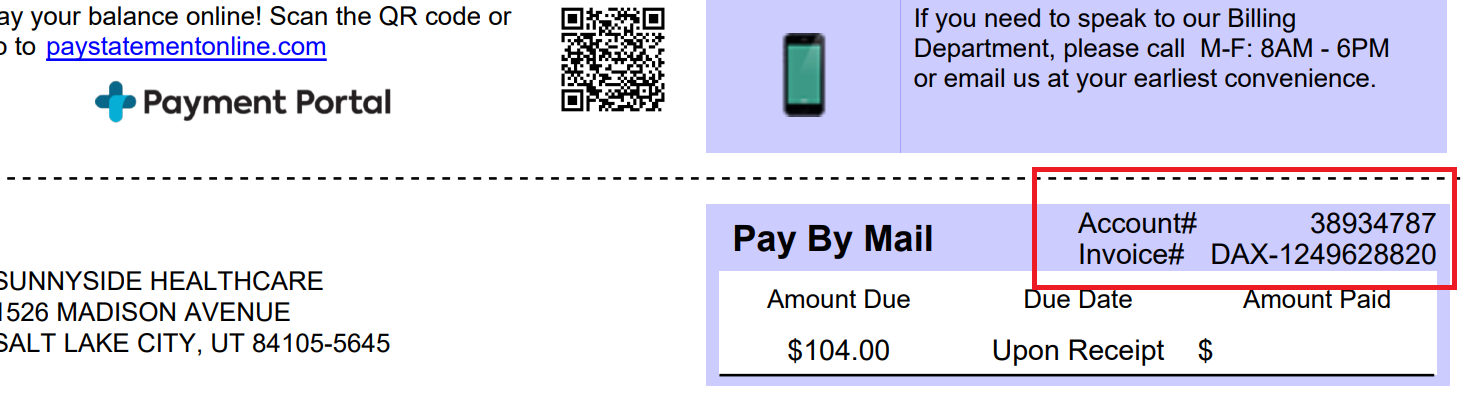
Within Statement Tracker, the system will show the Invoice # as it was sent on the statement (including any TCN Prefix) for Enhanced or Automated statements.
Please note that at this time Plain-Text Statements are not supported. For more information on setting up a Statement TCN Prefix, please visit our Add New Practice Help Article.
- Allow Entering Revenue Codes Longer Than 4 Digits: Updated Revenue Codes to allow entry of codes up to 9 digits, while only billing the first 4 digits. This enables users to utilize additional characters not billed for reporting, fee schedules, and contracts. It also provides the ability to have different defaults, such as modifiers and default units. For more information on adding revenue codes, please visit our Add a Revenue Code Help Article.
Patient
-
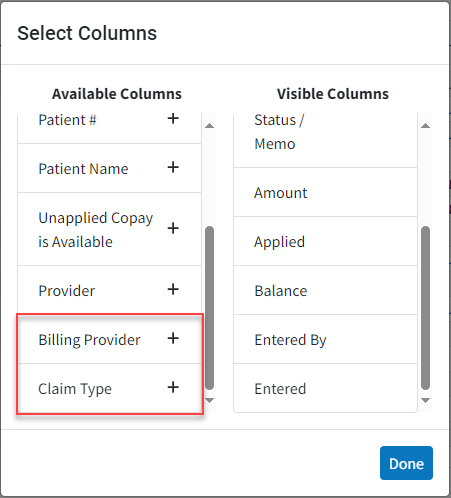
New Billing Provider and Claim Type Options for Manage Account and Activity Window: In this release, we added two new columns to the Manage Account screen (hidden by default). One for "Billing Provider" and "Rendering Provider" and one for "Claim Type." These columns will display values at the claim level but will remain empty for charges and credits.
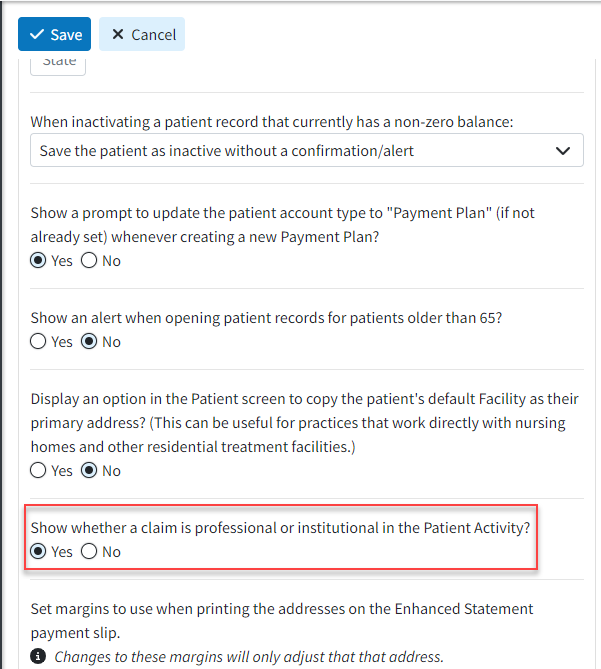
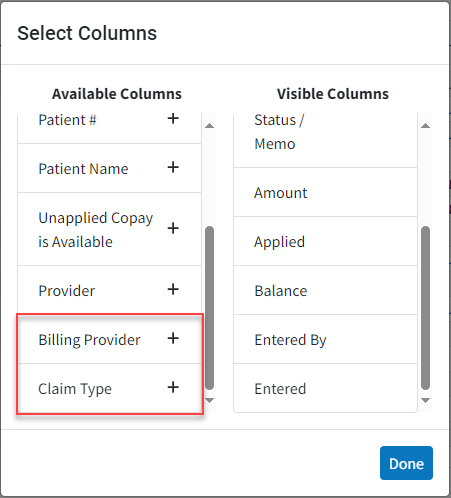 Additionally, we added a new Patient Setting called "Show whether a claim is professional or institutional in the Patient Activity?". When this setting is enabled, it will display whether the claim is professional or institutional by including either a (Prof.) or (Inst.) label after the claim number within the Claim Activity window.
Additionally, we added a new Patient Setting called "Show whether a claim is professional or institutional in the Patient Activity?". When this setting is enabled, it will display whether the claim is professional or institutional by including either a (Prof.) or (Inst.) label after the claim number within the Claim Activity window. 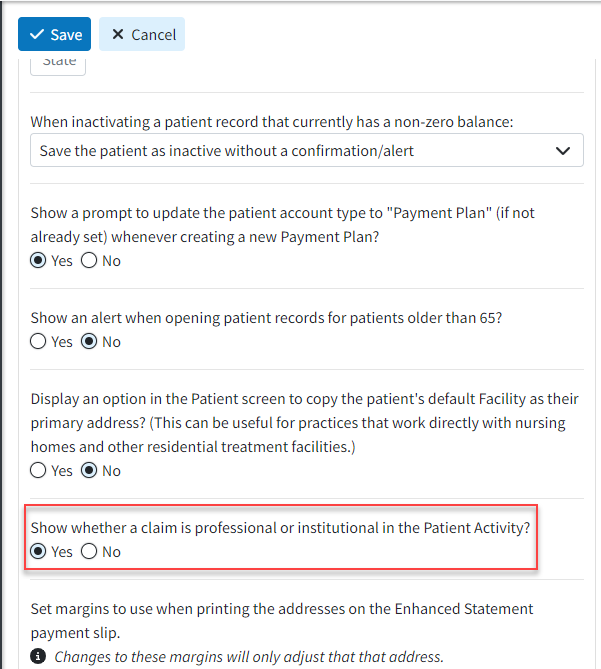
We have also modified the Activity Window to display the Billing Provider above the Rendering Provider in the claim listing if the Billing Provider is different from the Rendering Provider. Additionally, we have updated the label for the Rendering Provider to show as an Attending Provider if the claim is Institutional. For more information on this new Patient User setting, please visit our Configure Patient Settings for User Help Article.
Claim
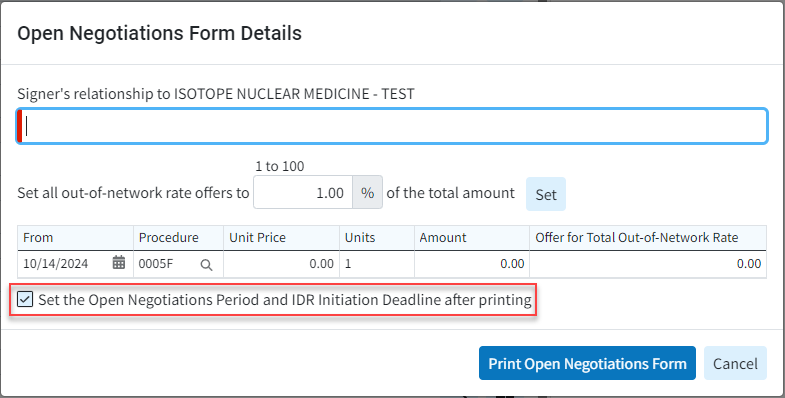
- New Ability to Store Relevant Dates When Sending Open Negotiations Form: Added the ability to store relevant dates ("Open Negotiations Period End" and Federal "IDR Initiation Deadline") when sending the Open Negotiations Form, making it easier for users to manage the Open Negotiations process. We included a new checkbox at the bottom of the Print > Open Negotiation Form screen to “Set the Open Negotiations Period and IDR Initiation Deadline after printing,” as well as a new "Open Negotiations" tab within the Claim Follow-Up Activity that will store this data.
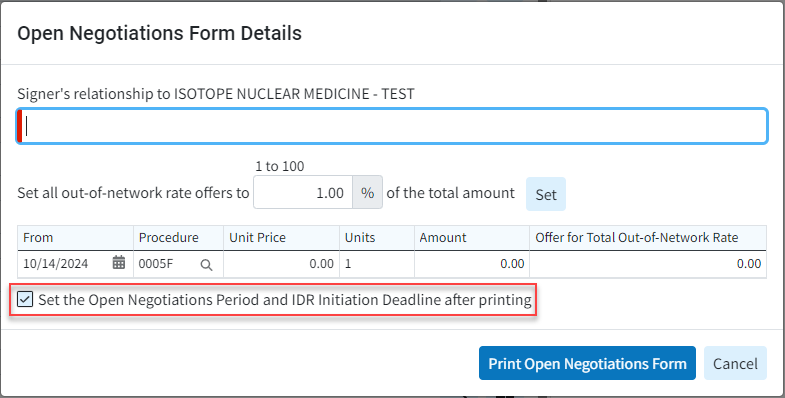
For more information on setting or managing the Open Negotiations Period and IDR Initiation Deadline after printing visit our Print Open Negotiations Form Help Article or our Manage the Open Negotiations Period and IDR Initiation Dates Help Article.
New Features and Updates
General
Customer Setup
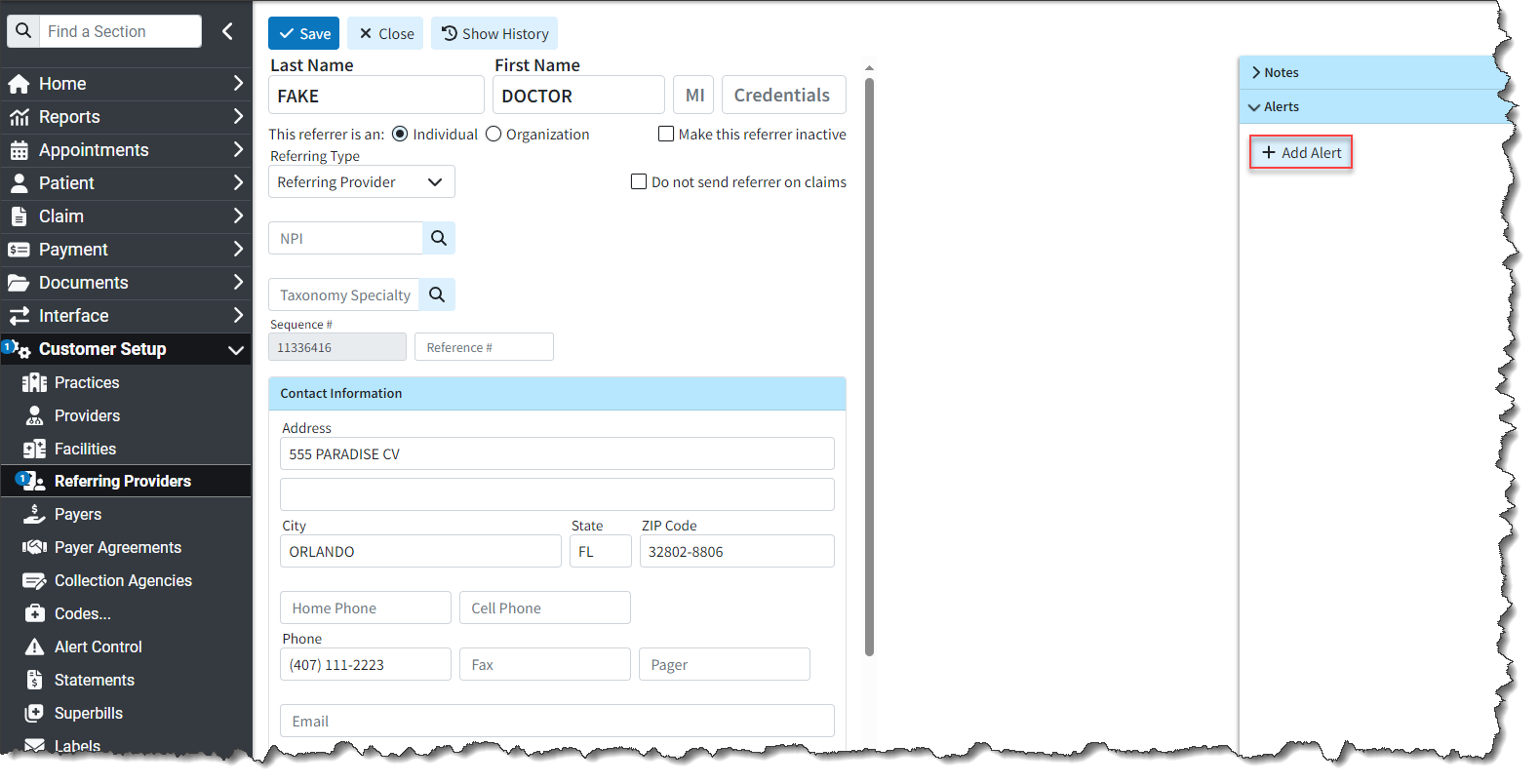
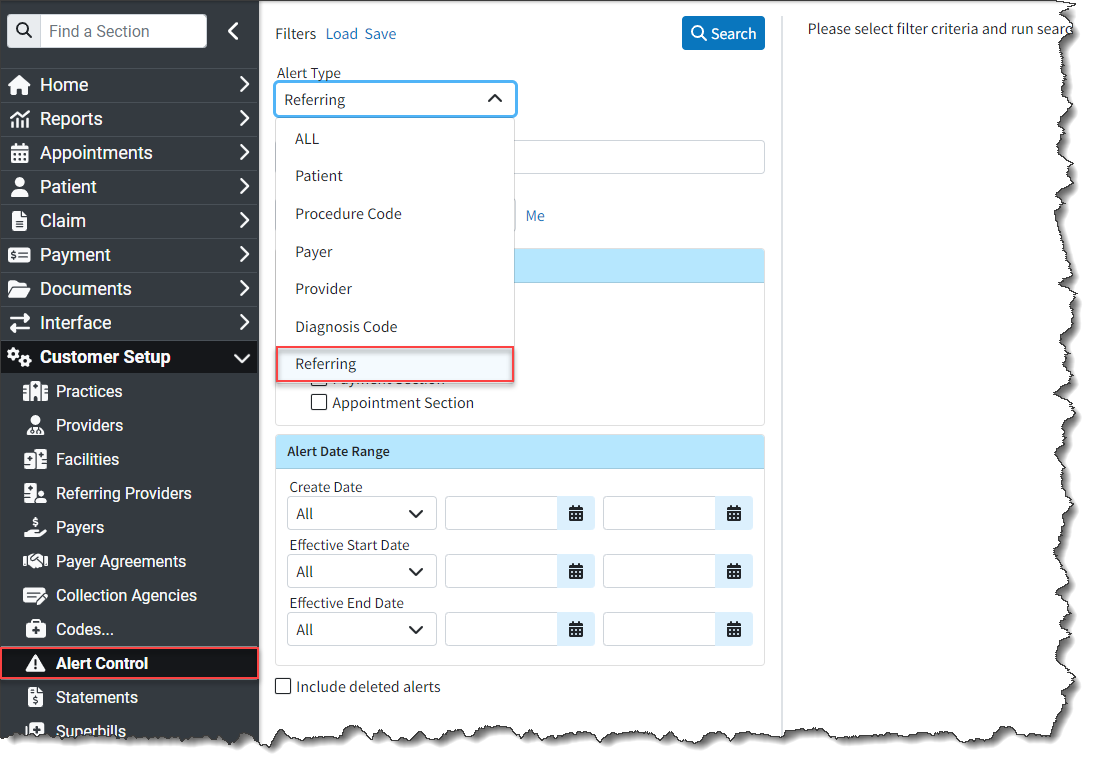
- New Referring Provider Alerts: We added the ability to create alerts for Referring Provider records. Previously, we only had alerts for payers, providers, patients, and codes. Users can now add specific alerts to their referring providers, which will appear as a pop-up whenever the referring provider is opened in specific sections of the CollaborateMD application. This will help ensure your team is aware of any important information associated with your referring providers/ordering providers/sales reps.
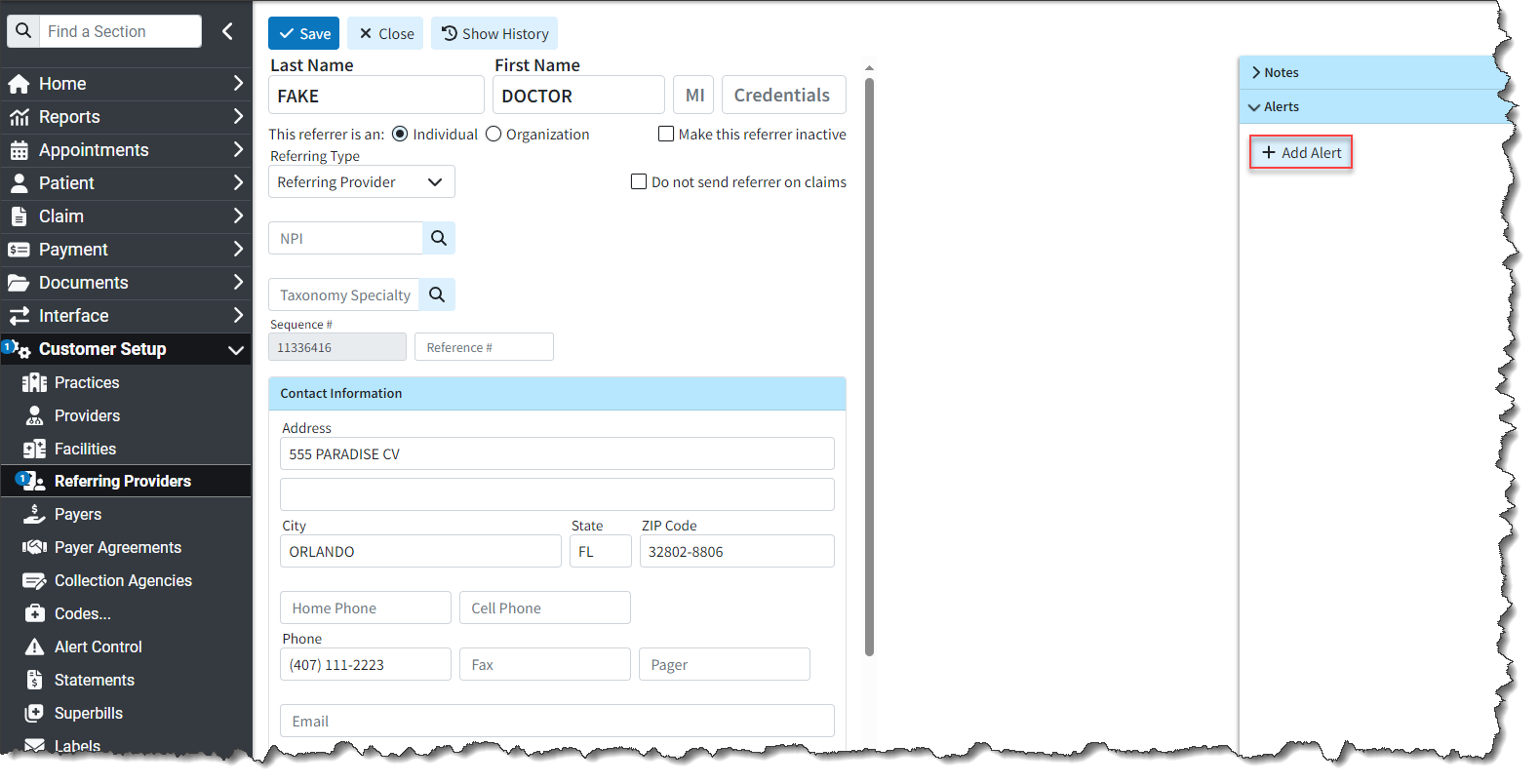
Additionally, we updated the Alert Control section to include Referring Provider as an option for “Alert Type” when searching for and displaying alerts.
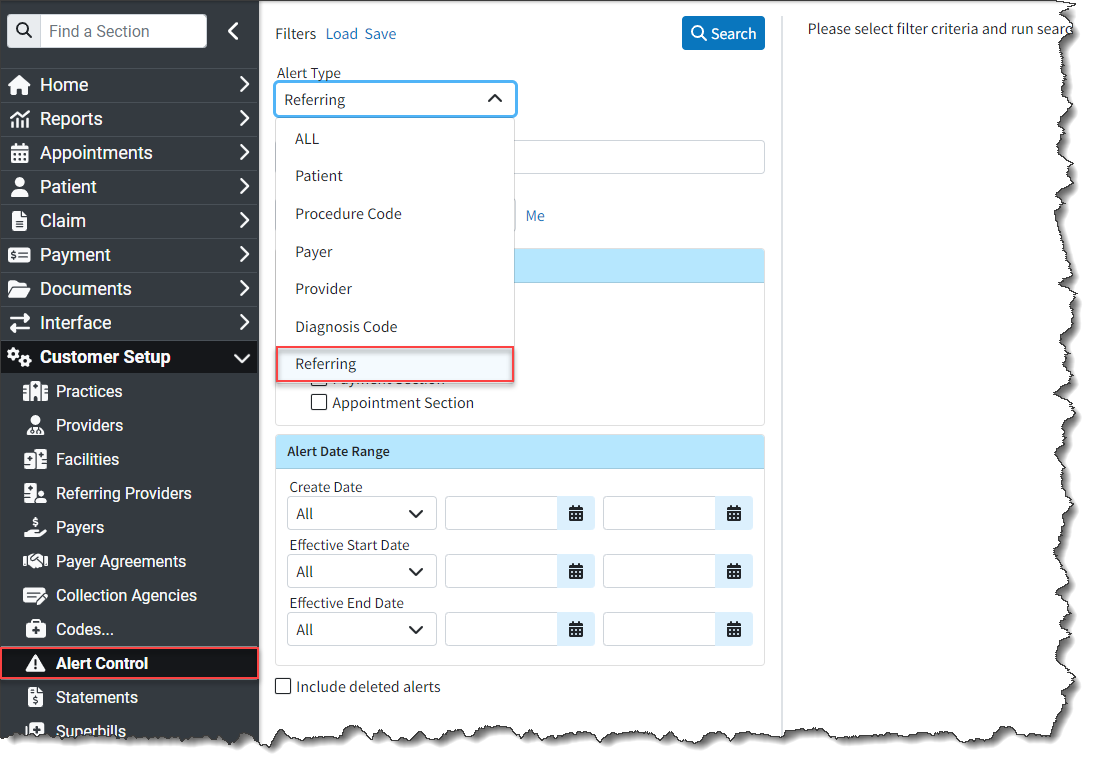
For more information, please visit our Referring Provider Alerts Help Articles.
Patient
- New Enhanced Auditing (Show History) for Patient: CollaborateMD has been working on a new enhanced auditing project that will provide offices with an easy and transparent way of auditing changes made in the application. We previously released our new Enhanced User Auditing feature in the Customer Setup section of the application, allowing users to see a detailed list of changes made to specific records throughout the application.
In this release, we are expanding our Enhanced Auditing functionality to the Patient section enabling users to track modifications, changes, and updates made to patient profiles within CMD for better auditing and accountability. With the new "Show History" feature, you can now determine which user changed specific Patient information in the software and when, by providing an auditing table with all updates or changes made to a record, including the user, date and time, and the item changed. 
These new auditing records are also included in our existing User Audit Report, making it an even stronger tool for auditing multiple records simultaneously. The Show History capability has currently been deployed in the Customer Setup and Patient sections, and we will be adding it to other sections of the application systematically.
For more information on using our new Add New Same/Similar Code List feature, please visit our Enhanced Auditing Help Articles.
Claim
- New Statement Counts in Claim Summary: When automated statement settings are set to "Separate by Claim," we don't show the Statement Count (mailed or electronic) in the Account Summary tab of the side panel. This is by design. However, we were not showing the statement count on the claim within the Claim Summary tab, causing the user to see only the total statements sent for each claim within the Manage Account screen.
In this release, we updated the Claim Summary tab to display statement counts, showing how many statements were sent for the claim when the statement separation setting is set to "Send separate statements for charges per claim" allowing users to see how many statements were sent for the claim.
Affected Statement Automation Setting:
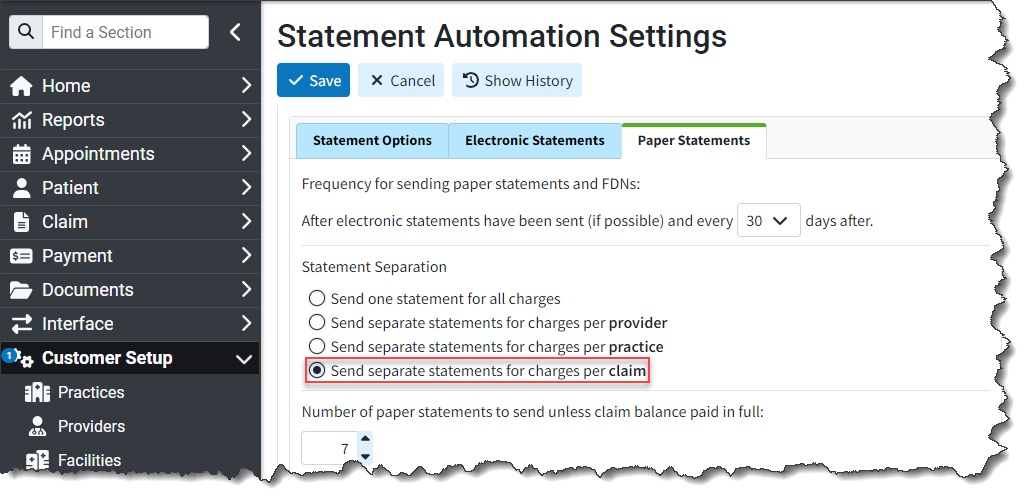
New Statement Counts Displayed in Claim Summary

New Features and Updates
General
Payment
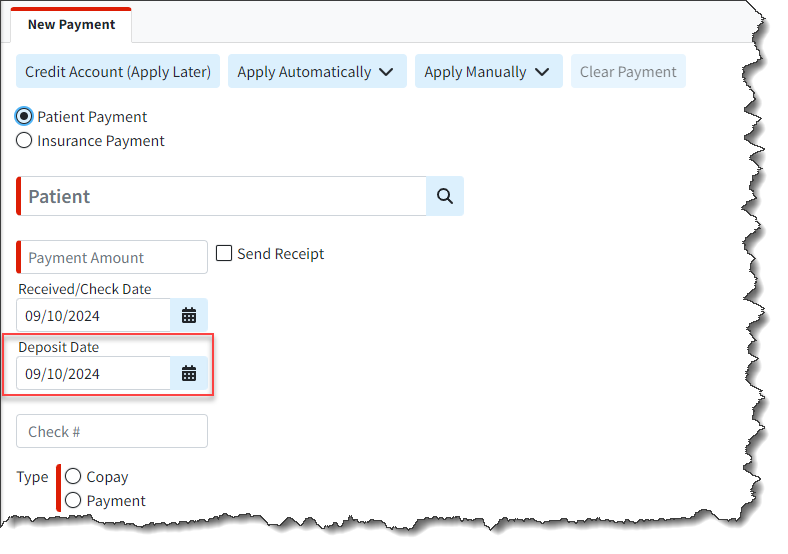
- New Deposit Date Field on Payments: We added a new "Deposit Date" field when entering or editing payments (ERA, EOB, or Patient Payment) to represent the date the check was deposited into the practice’s/provider’s account. This field will mirror the "Check Date" by default (for EFTs, it is typically the same as the check date) but can be manually changed if there are delays in ACH processing. This will help users who want to reflect any delays and match them with their bank statements.
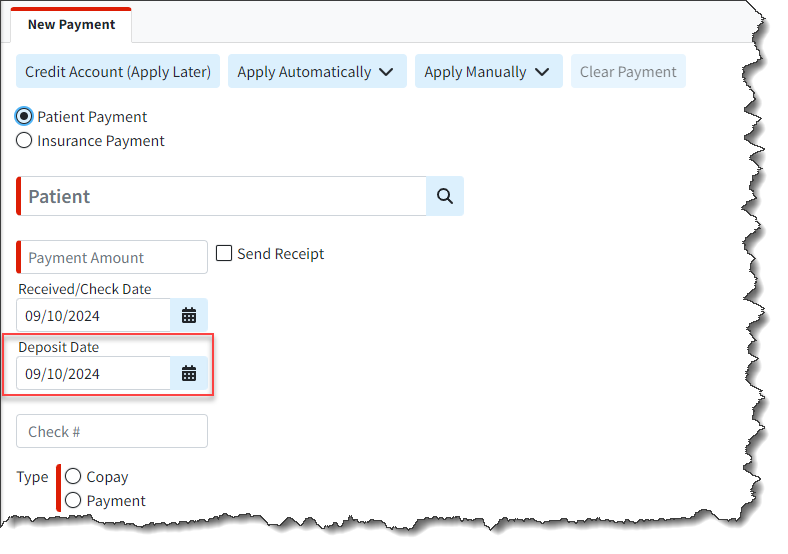
For more information on updating the deposit date, please visit our Post Insurance Payments Help Articles.
Patient
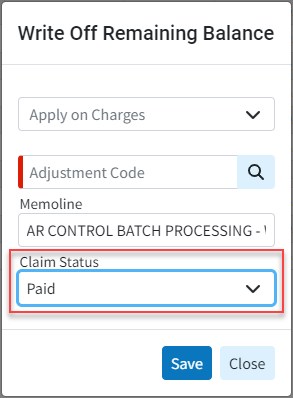
- New Option to Select Resulting Claim Status When Writing Off Charges: A new option has been added within Patient > A/R Control, allowing users to select the resulting claim status when writing off claims. The Write Off Remaining Balance dialog now includes an additional option for Claim Status, enabling users to choose any claim status, including custom ones.
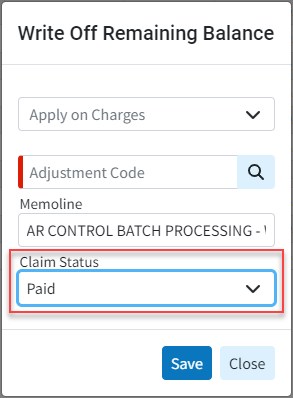
For more information on writing off charges, please visit our Write off Remaining Balance Help Article.
Claim
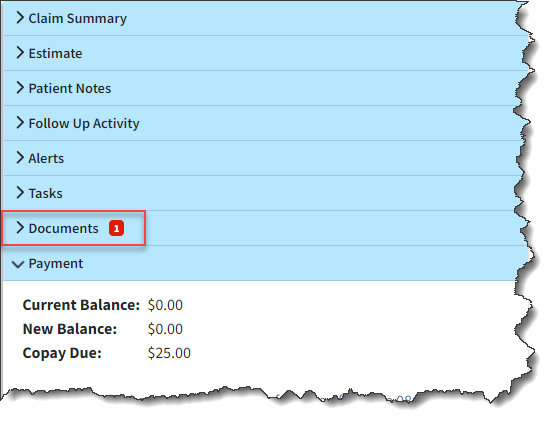
- New Indicator for Number of Claim Documents: Added an indicator for the number of documents associated with a claim or an ERA/EOB. This indicator is similar to our existing one for Patient Notes on claims and intake forms associated with a patient. It will display a red number on the "documents" button, indicating the number of associated documents.
View from the claim screen:
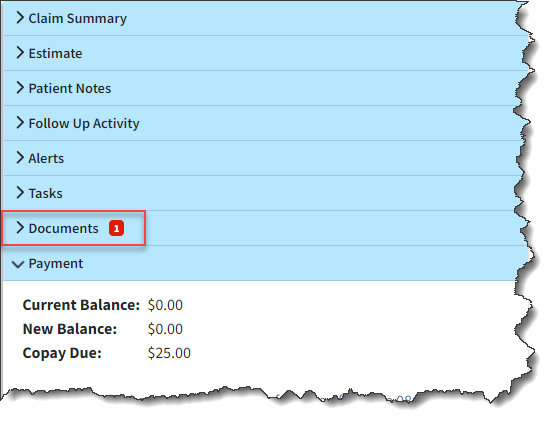
View from the Payment View Screen:

For more information visit our Manage Documents for a Claim Help Article.
Codes
- New Support of Value Codes as a Contract Parameter: Added a new checkbox option within Payer Associations for Contracts to support Value Codes as a contract parameter. When selected, users will have the opportunity to enter a single Value Code and Amount. The correct contract will be matched based on the Value Code and Amount (if present) when applying a payment. Please note that the system will continue to apply the contract that has the highest number of matching criteria.

For more information on using our new Contract Payer Association, please visit our Managing Payer Associations Help Article.
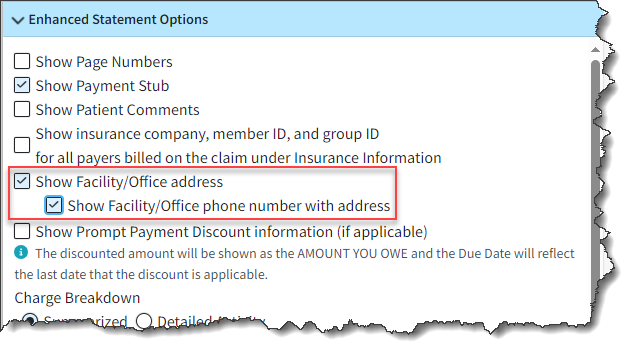
Statements
- Ability to Show Office/Facility Phone Number on Enhanced Statements: We previously added the ability for users to show the facility/office contact information on enhanced statements. In this update, we also added the ability to show the phone number for the office/facility within Enhanced Statements when the "Show Facility/Office contact information" box is selected.
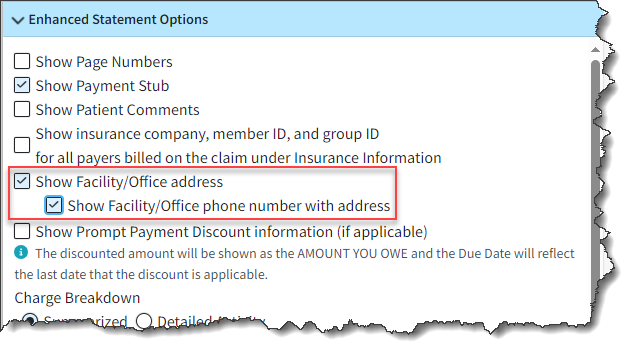
For more information on enabling enhanced statement options, please visit our Configure User Print Statement Settings Help Article.
Reports
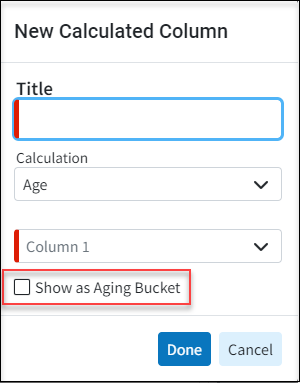
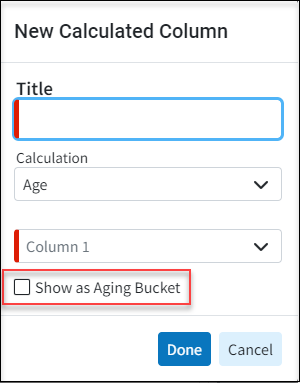
- Report Builder - New Age Calculation Option for Aging Buckets on Date Fields: We added a new checkbox option at the bottom of the Calculated Column dialog within the report builder that allows age calculations to show an Aging Bucket rather than the number of days.
- Report Builder - New Report Fields for Family Balances: Added the ability to report on the patient’s family balance by incorporating the following new report fields under Patient Data:
- Family Balance
- Family Patient Balance
- Family Insurance Balance
New Features and Updates
General
Customer Setup
- New Enhanced Auditing (Show History: CollaborateMD has been working on a new enhanced auditing project that will provide offices with an easy and transparent way of auditing changes made in the application. Our new Enhanced User Auditing allows you to see a detailed list of changes made to specific records throughout the application. This new auditing tool enables users to track modifications, changes, and updates within CMD for better auditing and accountability. With the new "Show History" feature, you can now determine which user changed specific information in the software and when, by providing an auditing table with all updates or changes made to a record, including the user, date and time, and the item changed. These new auditing records are also included in our existing User Audit Report, making it an even stronger tool for auditing multiple records simultaneously. The Show History capability has currently been deployed in the Customer Setup section, and we will be adding it to other sections of the application systematically

For more information on enabling or using our new Show History feature, please visit our Enhanced Auditing Help Articles.
Codes
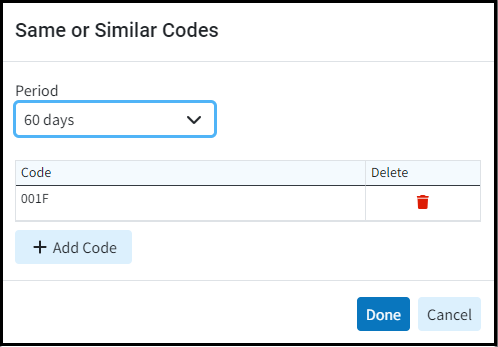
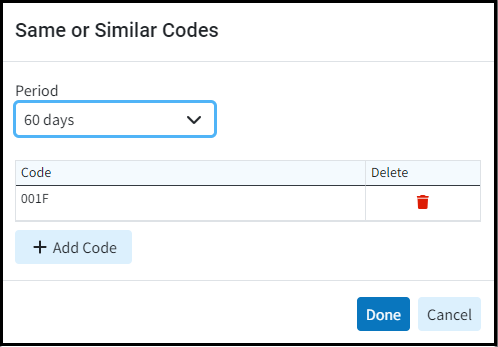
- New Same/Similar Code List Option: We added a new option within the Procedure Codes screen that allows you to capture “same or similar” procedures done within a specific time frame to warn users. This will allow you to add “same or similar” procedure codes that payers won't cover if billed within a specific timeframe. For example, Medicare only covers “routine foot care” (a.k.a. routine podiatry services) every 60 days. Adding these procedures to your Same/Similar Code List with a 60-day period will show a warning message when creating a new claim that falls within the period after a "same or similar" previously rendered procedure.
For more information on using our new Add New Same/Similar Code List feature, please visit our Add CPT/HCPCS Help Article.
Claim
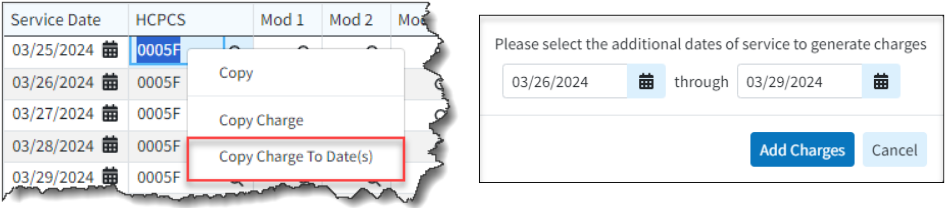
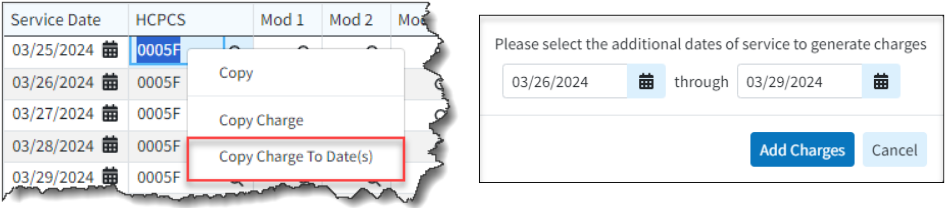
- New Copy Charges to Dates Option: To support users entering the same code multiple times for inpatient institutional claims (which are just the same HCPCS/Revenue codes for each day that the patient is in the hospital), we already offer "Copy Charge," a right-click option available in the Charge table. However, this still requires users to perform two clicks on each day for admit-through-discharge claims (which could be 10-20+ days). Additionally, users must update each charge’s date, as it copies them over with the same service date rather than advancing to the next day. We have added a new option to the right-click menu, "Copy Charge To Date(s)," allowing users to select a date range starting with the next DOS on the claim's charges. This option provides an editable date range to copy the charges to.
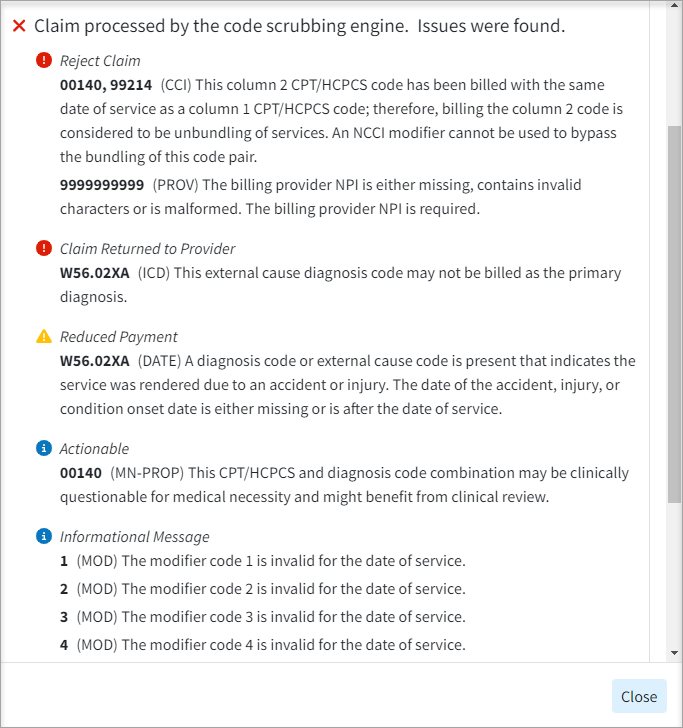
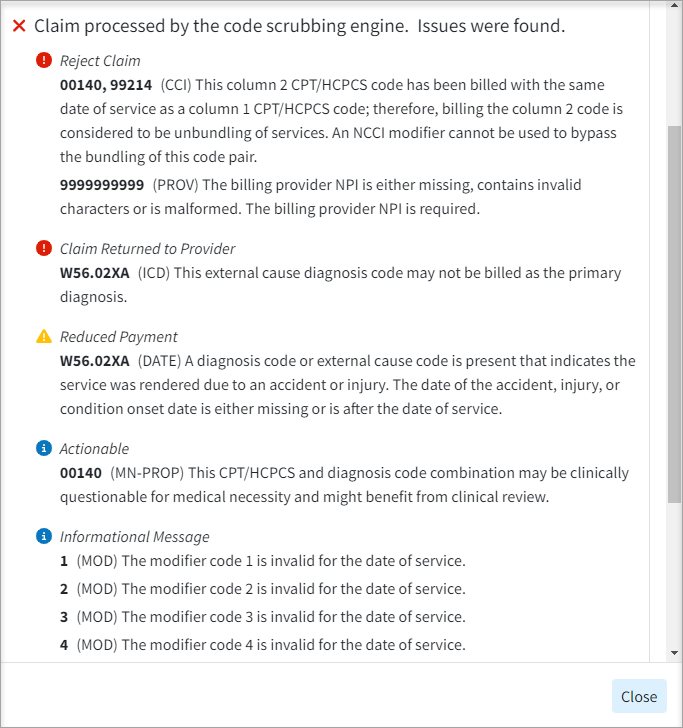
- Claim Review Results Screen Update: Updated the Claim Review Result dialog within claim scrubbing to sort the code scrubbing results by their severity (most severe on top) and show the associated message instead of calling them all “errors.”
Follow Up Management
- Update to the Follow Up Management Table: Added claim counts and balance totals to the bottom of the Follow Up Management screen.
New Features and Updates
General
User Bar
- New Option to Save the 'Open claim after searching'/'Open patient after searching' Options to User Preferences When Using Switch Customer: Updated the SysMgr/Switch Customer option to now Save the 'Open claim after searching' and the 'Open patient after searching' options as a User Preference.
Services
- Intake Forms - Added Formatting to Updox Form Field Values When Printing Forms: We previously added formatting to all Updox Form Field values in our web app. In this release, we added support to apply the same formatting that our Updox Form Field values have in our web app when printing forms.
New Features and Updates
General
Home
- New Timeline Item for Claims At Status: Added a new timeline item, "Claims At Status," which, when selected, provides a multi-select dropdown menu. This allows users to select one or more claim statuses, adding one entry to the daily section of the timeline for each selected status.
For more information visit our Help Article.
New Features and Updates
General
Claim
- New Option to Print EOB information When Batch Printing Claims: Added support for printing EOBs directly from Claim Batch Print. If any claims set to send to the secondary or tertiary insurance are selected when Print is clicked, the system will be given the option to print the EOBs.
For more information visit our Help Article.
Payment
- New Optional Column for Next Payer: Added a new optional column (hidden by default) within the Insurance Payment screen for "Next Payer" that will show what the next status will be based on the current payment and the payer priority (Secondary, Tertiary, Due Patient, etc.). This column will display who the next payer is in line for ERAs and Insurance Payments.
- Update to Save Additional Actions on ERAs When Using the Save And Apply Later Option: Updated the Save and Apply Later option within ERAs to now save additional actions when used. Any updates, such as changes to account credits, adjustments, debits, and info lines that previously weren't saved unless the payment was applied immediately, will now be saved, and the existing warning removed.
Customer setup
- Update to Remittance Codes Selected From the Master List: Updated the Remittance Codes so that previously added codes are grayed out and can't be selected from the Master List (just like we do with other codes).
New Features and Updates
General
Patient
- New Patient Notes Option to Allow filtering by date of service when Claim Notes is selected: Added a new filter button to Patient Notes > Claim Notes to allow filtering notes by Date Of Service.
By default, this filter will be set to "All."
- New email/text Receipt Feature: Added a new email/text receipt feature to help our customers achieve better and more efficient communication with their patients by enabling the sending of receipts via email or SMS. This will provide medical practices with greater flexibility and options for patients to receive their receipts in an effective and easy-to-understand format, enhancing patient comfort. As part of this project, our receipts will now offer a cleaner, more user-friendly, and easy-to-read format, along with more useful information when printing a patient receipt. Additionally, there is an option to print FSA/HSA receipts, which will include all the required additional information
For more information on our new Receipts, please visit our Help Articles.
- Patient Name Suffix Added to All Screens: Added the Patient Name Suffix everywhere the Patient Name is shown to make it easier for users to determine which patient is the correct one.
Claim
- New Option to Hide the Discharge Hour Field when the Claim Doesn't Involve a Discharge: Added an update to institutional claims to hide the Discharge Hour within the Additional Info screen when the third digit of the type of bill is 2 or 3, and the patient status is set to 30 (Still Patient).
Customer setup
- Added Remittance Code 23 to Warning When Adding an Action: We previously added a warning message to prevent users from adding remittance actions to common codes, because these actions are usually incorrect. In this case, we added code 23 to the list of common codes included in the warning message. We also added a new warning any time the Denial action is added to any code.
New Features and Updates
General
Reports
- New Report Fields: Added three new report fields under Claim Data to categorize claims by whether they have been paid or not. The fields are:
- Has Payment? Displays "Yes" if the claim has a payment associated with it. Displays "No" otherwise.
- Has Patient Payment? Displays "Yes" if the claim has a patient payment associated with it. Displays "No" otherwise.
- Has Insurance Payment? Displays "Yes" if the claim has an insurance payment associated with it. Displays "No" otherwise.
All three have multi-select filters with options for “Select All”, “Yes”, and “No” when added as a filter.
Appointments
- New Intake Form Icons in The Scheduler Added a new right-click option from the scheduler to send forms that have not been sent without having to open the appointment. We also added a right-click option to Apply Forms that have been sent, but not applied.
Furthermore, we added icons to appointments within the scheduler to indicate the status of the forms:
 | The appointment is for today or later and forms have not been sent or submitted |
 | Intake forms were sent, but the patient hasn’t filled them out yet |
 | Intake forms have been submitted and are ready to apply |
 | Intake forms were applied |
No Icon | The appointment is in the past and forms were not sent or submitted |
Claim
- New Search options within Follow up Management: Added the ability to search Date of Service and Follow-Up Date by the number of days within Follow-up Management. The new "# of days" filter option will now control all date ranges, similar to how the Patient A/R Control filter is set up.
Payment
- New Ability to Allow Changing the Action Dropdown on ERAs: Enabled the Action dropdown when reviewing ERAs, allowing users to manually change the Action to Denied so that the charges are set as a Denial (this is still disabled when viewing the Apply report or when viewing a check without editing permissions).
- New Ability to Allow Filtering by Issue Type on ERAs: Updated the ERA results screen to include multi-select dropdowns in place of the existing Errors, Warnings, and Information checkboxes. These dropdowns allow users to filter by specific errors, warnings, or information messages present in the report. Each dropdown only contains a list of issues that are found in the current report.
Customer setup
- New Setting to Send the Patient Address in Box 32 for Place of Service 12: Added a new checkbox option under Payer → Billing Options → General → Professional. When selected, the option to "Send the Patient Address in Box 32 for Place of Service 12" will replace Box 32/Loop 2310C with the patient’s home address instead of the facility when the professional claim's POS is 12.
New Features and Updates
General
Claim
- New Productivity Reporting: Added a new Claim Status button to the claim screen (between the Activity and More buttons). When clicked, it will provide options for:
- New Claim Status Check
- Last Checked On mostRecentStatusCheckDate()
- View All Past Claim Status Reports
The "New Claim Status Check” option works exactly as the More → Claim Status button works today, including ensuring that the claim is "At Insurance" and showing a dialog if the status was already checked today.
Referring Provider
- New Columns Within the Referring Provider"Show All" List: When looking up a referring provider, you may be doing so based on a fax, phone call, or email. Therefore, it would be helpful to have additional optional columns in the "Show All" Referring screen with this information. We added the following columns to the referring provider "show all" table that will be hidden by default:
- Home Phone
- Cell Phone
- Fax #
- Added New Referring Label Fields: Added new fields to the Referring Label options when creating a label:
- Home Phone
- Cell Phone
- Fax #
- Pager
- Email
- New Referring Provider Data Report Fields: Added the following new report fields to the Referring Provider Data:
- Home Phone
- Cell Phone
- Fax #
- Pager
- Email
User Management
- New Download Snapshot Permission: Added a new permission to the Account Administration section. This new "Download Snapshot" permission is required to use the Download Snapshots button under the User Profile menu and will have two levels:
- Deny: The user cannot download one-time or recurring snapshots
- Allow: The user can download one-time or recurring snapshots
Note: For users with a "Role" assigned, an Auth Rep or Admin not associated with a role must update the permission to "Allow" for user to be able to download snapshots.
New Features and Updates
General
Dashboards
- New Productivity Reporting: Added a new Dashboard Gadget and 3 new reports to provide our customers with the ability to report on the productivity of their users:
- Dashboard Gadget: Average Touches to Completion - A new dashboard gadget will display the average number of times a completed claim with a balance of $0.00 was worked, based on either the claim notes or follow-up notes. The new gadget will be visible to Management users on the Welcome screen.
- Report: User Productivity by Notes - A new report that shows the number of Notes(claim notes and claim follow-up notes) that have been created by each user during the specified time frame.
- Report: User Productivity by Tasks Assigned - A new report that shows the number of tasks assigned by a user during a specific time frame.
- Report: User Productivity by Tasks Completed - A new report that shows the number of tasks completed by a user during a specific time frame.
Patient
- New Columns Within the "Recently Opened List": Added three new columns to the "Recently Opened" list within the Patient, Manage Account, and Claim screens. The newly available columns are Facility, Provider (already available in the Claim section), and Primary Insurance (Payer Name). These new columns will be hidden by default.
Codes
- Update to the "All Inclusive" Option for Procedure Codes: Updated the Procedure Codes to allow setting "All Inclusive" codes that send other charges as $0.00 or $0.01. When the option “This is an all-inclusive code” is selected in the Procedure Codes section, the system now displays a dropdown box with new options. Upon selection, the Claim section will set all other charge amounts to $0.00/$0.01, making the amount field non-editable.
Intake Forms
- Ability To Reorder Intake Forms: A new column with a drag handle has been added under Services > Intake Forms, enabling users to reorder the forms and determine their sequence (order) as they appear to patients within the forms portal.
- New Timeline Item for Unapplied forms: Added a new Timeline item titled "Forms Ready to be Applied," which displays the number of non-deleted appointments from the past seven days (including today) where patients have submitted intake forms that have not yet been applied.
New Features and Updates
General
Dashboards
- Update to the Lag Time Gadget's Averages Displayed Terminology: We updated the terminology of the averages displayed at the bottom of the Lag Time Gadget to better align with what most providers are seeking. To enhance their understanding, we renamed the "Total Average Lag" metric to "Average Time to Payment," which indicates the average lag time from when the charge occurred to when it was paid. Additionally, we changed "Billing Lag" to "Charge Capture Lag," reflecting the average time from when the charge occurred to when it was billed to insurance, and introduced a new benchmark:
- Above Average: 1 day
- Average: 2 days
- Below Average: 3 or more days
Tasks
- Update to Show The User Who Assigned a Task: We updated the Tasks section and added the ability to display the person who assigned a task, rather than just the creator of the task. This allows users to reassign tasks to the assigner if clarification is needed. Please visit our Help Article for more information on adding or editing a task.
Reports
- New "Between" Filter Option for Text Fields on Reports: When filtering a report by names, users may need to split the report based on a range of the first letters of the names. To aid in this, a new "Between" option has been added to all report text filters, allowing users to filter names by a range of first/last name letters (e.g., A-G, H-N, etc.), facilitating better task assignment. Visit our Help Article for more information on adding report filters.
Patient
- New Ability To Save Credit Card Information: We previously allowed patients to securely store their credit card information as a payment profile within the payment portal by selecting the option to “Save my payment information for next time.” However, this convenient feature was not accessible within the application until now.
With cardholder consent, payment (Credit Card) information can be saved for future payments. Users can now save payment (credit card) information when processing patient payments, allowing them the convenience of managing saved cards directly within CollaborateMD by checking the new “save my payment information for next time” box. Users will also be able to save and manage payment information directly from the patient section.
This enhancement aims to streamline the payment process and offer users greater control and flexibility in managing their payment methods. Please visit our Help Article for more information on saving payment information.
ERA
- New Option To Allow Users To Filter ERAs By Specific Error/Warning/Message: We updated the ERA results screen to include multi-select dropdowns in place of the existing Errors, Warnings, and Information checkboxes. These dropdowns allow users to filter by specific errors, warnings, or information messages present in the report. Each dropdown only contains a list of issues that are found in the current report.
New Features and Updates
General
Reports
- New First Pass Resolved Claims Standard Report: A new standard report, "First Pass Resolved Claims," has been added. It is linked to the First Pass Resolution Rate Gadget as a drill-through option and will generate a list of claims comprising the first pass acceptance rate.
- Update to Report Viewer to Remember User Preferences: Added support to the report viewer to remember user preferences for Standard, Custom, and Hidden reports upon loading the app, instead of resetting them to Standard and Custom each time.
- New Report Fields and Category For Claim Validation Charges: Added support to the report viewer to remember user preferences for Standard, Custom, and Hidden reports upon loading the app, instead of resetting them to Standard and Custom each time.
Appointments
- New Patient Intake Forms Feature (Beta): Added a new Patient Intake Forms feature that enables users to create forms (through Updox) that can be automatically sent with appointment reminders or manually dispatched. The form data is received as discrete fields, which can then be entered into our application. This reduces the potential for errors and increases automation in the patient check-in process. Please note this feature is still in the Beta stage. Please visit our Help Article for more information on Patient Intake Forms.
New Features and Updates
General
Claim
- Update to The "Offer For Total Out-Of-Network Rate" In The Open Negotiations Form: Updated the Open Negotiations Form to allow setting the "offer for total out-of-network rate" for each charge individually, as well as setting all the out-of-network rate offers based on a percentage (1% to 100% ). Visit our Help Article for more information on printing Open Negotiation Forms.
Providers
- New Facility Claim Default Option Added to Provider Records: A new Facility option has been added within the Provider > Claim Defaults section that will automatically send the facility information on claims created for the rendering provider but that does not have a facility assigned (whether sent via interface or set as patient default facility).
New Features and Updates
General
Report Builder
- New Warning For Aggregated Columns With Too Many Report Connections: Added a new warning to the report builder that alerts the user when an aggregated column—or a column set to display totals—may not show the expected values due to the report field having too many relationships (connections).
Claim
- Update to The Charge-Specific Rendering Provider Option on Claims: We have updated the Charge-Specific Rendering Provider option on claims (Claim > Charges > Other Info) to reduce confusion when selecting a different provider for each charge. With this update, users will be prompted to indicate if the service was rendered by a different provider than the one associated with the rest of the claim. If "No" is selected (the default option), no provider will be shown. If "Yes" is selected, the Rendering Provider dropdown will become available. Visit our Help Article for more information on updating the rendering provider on a charge.
Claim Follow Up
- New Option Within Claim Follow-Up to Update Claim Status: A new option has been added to the Claim Follow Up Management that allows for manual changes or updates to the claim status. This update introduces a dropdown option that functions similarly to the "Set all charges to" feature in the claim section.
Payment
- New Option to Allow to Apply Interest Adjustments Amounts to Claim Balance: A new payment setting has been added for users to "Automatically post interest amounts as payments," which will reduce the claim balance owed by subsequent payers and the patient. This enhancement allows users to apply interest adjustment amounts to the claim balance. It also includes a new column "Apply to Claim Balance" that will be displayed when linking a claim to a provider-level adjustment, enabling users to apply the provider adjustment to the claim balance (Interest amounts must be equal to or less than the balance itself). Visit our Help Article for more information on turning on this setting.
New Features and Updates
General
Report Builder
- New Warning Indicator When a Report Field is Added Multiple Times: A new indicator has been added to the report builder that shows a warning when the same field is added multiple times. This update introduces an icon next to the field within the column list, accompanied by a tooltip indicating that the field is already in the report. Additionally, we have included a new Report Setting titled "Show an indicator when duplicate columns are present in the Report Builder," which can be toggled on or off. Please visit our Help Article for more information on toggling this setting.
Scheduler
- New Option for Blocks and Block Templates to Allow/Prevent Overbooking: A new option has been added to Scheduler Blocks and Block Templates that enables or disables the ability to schedule multiple appointments at the same time (overbooking) during a specified block. When this option is set to block overbooking, it will prevent users from scheduling appointments during that block even if their scheduler settings are configured to allow overbooking. Visit our Help Article for more information on adding a block template.
Interface
- New Option to Batch Import 837 Files: We have added the ability to manually batch-import claims into the application by loading 837 files directly from the Interface > Import section, similar to the HL7 import. This feature enables users to search for claim messages via the interface tracker after the ANSI (837) import and locate their claims within Status Control after a successful import for review and submission. Visit our Help Article for more information on importing ANSI (837) Files.
Invoices
- New Invoice Print Option: We have added the ability to print either a detailed or summarized invoice from the Invoice History screen. Users can now print a summary PDF, similar to what is emailed to them, directly from the right-click menu. The Print option at the top of the Invoice Details screen will continue to print the detailed version of the invoice.
New Features and Updates
General
Dashboards
- Update to The First Pass Resolution Rate Gadget Calculation: We Updated the calculation within the First Pass Resolution Rate Gadget to exclude the last 14 days when viewing the Last 30 Days, and the last 30 days when viewing the Last 90 Days or longer. This will provide a more accurate FPRR, as the most recent days do not provide useful information because claims that were just submitted have not yet been paid and are therefore not resolved.
- New Report Fields Added Ahead of New Report for FPRR: Added new report fields related to the First Pass Resolution Rate (FPRR) in preparation for an upcoming new Standard Report:
- Claim Data → Primary Payer → Allowed Amount
- Claim Data → Primary Payer → Times Billed
- Activity Data → Claim Activity → Payer Priority
- Activity Data → Claim Activity → Is First Submission?
- Activity Data → Claim Activity → Is Resolved on the First Pass?
Eligibility
- Patient Eligibility Report Table Improvements: We Improved the Patient Eligibility Report table by removing the redundant Service Types column, as there is already a Service Type column included. We also enhanced the view for rows with more than 12 lines of services. Previously, only the first 12 service lines were displayed. Now, the first 11 lines are shown with a link to "Show All (X Types)" at the bottom, which opens a dialog with the full list of service types.
Claim
- New Option to Print Open Negotiations Form: Added a new print option within the Claim section that will allow a user to print an Open Negotiation Form (OMB 1210-0136) directly from the claim screen so that providers that are out-of-network can enter open negotiations with the insurance company to determine the amount that the insurance company will pay for emergency services. Please visit our Help Article for more information.
- Claim Summary Side Panel Update: Updated the Claim Summary (side panel) within the Claim Charges tab to automatically expand when the screen is wide enough (1440p, or 2560 x 1440 and above, or equivalent). Screens that are not wide enough will still automatically have the side panel collapse.
ERA
- New Option to Delete Multiple ERA Files at Once: A new button has been added at the top of the ERA search screen, enabling the deletion of multiple uploaded ERA files simultaneously. The "Delete ERA Files" button will be visible only if at least one ERA in the search results is eligible for deletion. This feature allows users who accidentally upload multiple unwanted ERAs with a method to remove them without the need to delete them individually.
Providers
- Update to Identify Providers With an Existing Submitter ID: Updated the application so that when a new NPI (Provider) is saved for an existing Tax ID (Submitter ID), we will now use the Submit Facility endpoint at the time the provider is created, rather than waiting until an agreement is started. This will allow ePS to register the NPI as associated with the current submitter ID and enable work on an ERA split before an ERA arrives.
Payers
- Update to The "HMO Medicare Risk" Payer Type Name: We Updated the Payer Type name from "HMO Medicare Risk" to "Health Management Organization (HMO) Medicare Risk (Medicare Advantage)" within the Payer section to better represent its purpose. This option will now appear in the Payer Type dropdown menu under the new name. For more information on setting up payers, visit our Help Article.
 Additionally, we added a new Patient Setting called "Show whether a claim is professional or institutional in the Patient Activity?". When this setting is enabled, it will display whether the claim is professional or institutional by including either a (Prof.) or (Inst.) label after the claim number within the Claim Activity window.
Additionally, we added a new Patient Setting called "Show whether a claim is professional or institutional in the Patient Activity?". When this setting is enabled, it will display whether the claim is professional or institutional by including either a (Prof.) or (Inst.) label after the claim number within the Claim Activity window.