New Features and Updates
General
Claim
- New Option to Select a Different Rendering Provider on a Charge: Added a new Rendering Provider dropdown field under Claim → Charges → Other Info → Service Information. This option will allow users to send a different Rendering provider for each charge (Box 24J / Loop 2420A). This field will make it possible to send a different Rendering provider for each charge individual charge. Please visit our Help Article for more information.
Claim Tracker
- New Claim Tracker Status Type: We added a new Tracking Status Type for “Unprocessed” within Claim Tracker. When selected, claims with a status of unprocessed (claims not acknowledged by the clearinghouse) will be shown in the tracking results. For more information on tracking statuses visit our Help Article.
Payers
- New Payer Billing Option to Print Supervising Provider in Box 31: We added a new Payer billing option under Payer → Billing Options → General → Professional section that will print the Supervising Provider in Box 31. This will allow customers sending Medicare claims to be able to include the Supervising Provider’s Name and credentials in Box 31. For more information on setting up this billing option, visit our Help Article.
New Features and Updates
General
Payers
- Automatically Adjust PR~45: We added a new option within the Payer → Billing Options → ERA screen to adjust the PR~45 (patient responsibility adjustment due to a contractual overage) when an ERA is posted, rather than setting it as Unpaid. This will allow providers who prefer not to charge this extra amount to the patient to have it automatically adjusted in our system. Please visit our Help Article for more information on turning this billing option on.
Interface
- Manually Import HL7 Files: We added a new interface option that allows customers to upload files and manually import claims into our system as HL7 interface messages (just as they would if they were sent through the WebAPI or any other interface). This will allow users to immediately run a search in Interface Tracker showing the messages that were just imported. For more information on manually importing HL7 files visit our Help Article.
New Features and Updates
General
Account Administration
- Password Reset Email timeframe extended: We understand that sometimes Admins/Auth Reps have to reset user passwords for users who might not be in the same office or even in the same time zone. This could be an issue since the password reset emails would expire after 30 minutes making it difficult for some users to reset their password on time. We've now updated the user password reset emails to be valid for the same length of time as our welcome email (24 hours) instead of the 30-minute default. This will allow users enough time to reset their password without having their email link expire.
For more information about resetting a user password, please see our Help Article.
New Features and Updates
General
Patient
- New Patient Account Summary Option: We added a link in the Patient Account Summary side panel ( for patients that have a “Family Account Type: Dependent”) that shows the master patient’s name and patient ID, with the patient ID being a link to open that patient. This will make it easier to identify the master patient when viewing the patient within Manage Account or the Appointment section.
ERA
- New Option to Upload Multiple ERAs at Once: It's easier than ever to upload ERA files received manually! We have updated our ERA file upload to allow users to select multiple 835 files to upload at once. This will allow you to upload many ERAs at the same time instead of one by one, saving you time and helping auto-apply files faster.
For more information about manually uploading ERAs, please see our Help Article.
New Features and Updates
General
Dashboard
- New Dashboard Gadget: Lag Time: A new dashboard gadget is now available in the Dashboard section, Lag Time.
Lag Time shows how long, on average, a charge will spend in each part of the revenue cycle (charge lag, insurance billing lag, and patient billing lag). Understanding charge lag is the key to understanding where to invest in efficiency within your practice. An average billing lag (the number of days between the date of service and billing the insurance) should be between 1-3 days.
A new report, Lag Time, has also been added.
For more information about the Lag Time gadget, please see our Help Article.
Dashboard
- New Dashboard Gadget: First Pass Resolution Rate: A new dashboard gadget is now available in the Dashboard section, First Pass Resolution Rate.
The First Pass Resolution Rate calculates what percentage of claims are paid on the initial submission. This metric captures your overall efficiency through all clearinghouse and payer edits/rules. The typical average net collection rate is 80% or more. The top practices aim for an FPRR of over 90% to ensure you maximize the efficiency of your revenue cycle!
For more information about the First Pass Resolution Rate gadget, please see our Help Article.
Dashboard
- New CMD Default Dashboard: The CMD Default Dashboard in the Dashboard section has been enhanced and updated to deliver even more real-time visibility and data into the financial performance and health of your account so you can easily measure your account's health and productivity.
Everyone needs good reporting metrics and CollaborateMD knows that many customers often rely on our default metrics and workflows (like our default dashboard). With that in mind, we have improved the CMD Default Dashboard to include more of the metrics that are important to our customers. To ensure that our users have access to this valuable information, the CMD Default Dashboard now includes the following gadgets: 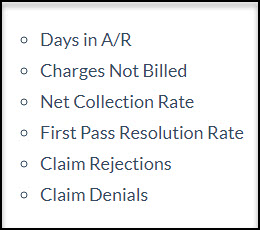 As part of this release, we updated the default dashboards shown on the Welcome Page to display our new gadgets for any welcome page roles selected. We also made all our new dashboard gadgets available for custom Welcome pages.
As part of this release, we updated the default dashboards shown on the Welcome Page to display our new gadgets for any welcome page roles selected. We also made all our new dashboard gadgets available for custom Welcome pages.
For more information about our Dashboards and Gadgets, please see our Help Article.
New Features and Updates
General
Codes
- New Situational Modifier Option: We know that some modifiers are specific to the type of provider performing the service. For example 80 (Assistant Surgeon), AF (specialty physician), AJ (clinical social worker), etc.
CollaborateMD has added a new situational modifier option within the Procedure Codes section that will allow you to add situational modifiers by Specific Rendering Provider Credentials (the credentials field in the Provider section).
When this option is selected and the Rendering Provider Credentials are entered, it will add the situational modifier when the credentials entered on the claim match the credentials of the Rendering/Attending provider set on the modifier.
For more information about setting up new Situational modifiers by specific Rendering Provider Credentials, please see our Help Article.
Codes
- Automatically Include Amount in the Memolines: We've added an enhancement to our existing option to “Use the Memoline on the Activity and Statements” within the Remittance Codes section. This enhancement will allow you to select an option to “Include the amount in the memoline.”
Once selected, when a remittance code is added (either in a manual insurance payment or an ERA) the info line that is included in the statements and activity will now display the amount associated with the code at the end of the info line.
New Features and Updates
General
Patient
- New Save and Reopen Option in Manage Account: When adding a credit or a debit to a patient record within Manage Account it is sometimes necessary to save, and then reopen the patient to take additional actions. The new
 button within Manage Account now allows you to save your changes and automatically close and reopen the screen loading the same patient record. This allows the user to create a credit/debit or action and then immediately act on that item without having to manually reopen the patient record.
button within Manage Account now allows you to save your changes and automatically close and reopen the screen loading the same patient record. This allows the user to create a credit/debit or action and then immediately act on that item without having to manually reopen the patient record.
Interface
- Interface Tracker: New Payers Filter Option: The Interface Tracker has been updated to include a new “Payers” filter option. This new filter allows users to filter interface messages by a specific Payer or Payers. This update also added a new column within the results screen for the payer that was sent in the interface message.
Please Note: That the payer search field and column will only work for interface messages sent after the release of this field. Messages received prior to this release will not match the payer filter or show the payer information in the column.
New Features and Updates
General
Dashboard
- New Dashboard Gadget: Net Collection Rate: A new dashboard gadget is now available in the Dashboard section, Net Collection Rate.
Your net collection rate indicates what percentage of your net charges (your charges less contractual adjustments) your practice is collecting. This is a powerful indicator of your practice's revenue cycle efficiency. The typical average net collection rate is 95% or more. The top practices aim for 99% net collections!
A new report, Daily/Monthly Net Charges, has also been added. You can also use the Net Amount report field in the Charges Data section in your own custom reports!
Please Note: To ensure that all users have access to this valuable information, and to allow all users to view data for all time, the data for the Net Collection Rate gadget is updated once per day. Changes made during the day will not reflect on this gadget until the next day. Please run Reports if you need up-to-the-minute data.
Payment
- ERA Credit Card Payments: Some payers are starting to send their payments by Credit Card (for example, using VPay), and as of this release, you can now process those credit card payments at the same time that you apply the ERA -- just click the Edit button and change the Source to Credit Card while you're reviewing the ERA. When you apply the payment, you'll be asked to enter the credit card details.
This feature is available for users of our In-App Payment Processing feature. If you want to take advantage of this time-saving integration, have your authorized representative start the process in the Services section today.
New Features and Updates
General
Reports
- Denial Reporting Updates: The Denials report and the Is Denial? report filter have been updated to better reflect all of the denials that you have received and enable a complete understanding of your Denials, including partial denials.
The updated Denials report will now show adjustment codes rather than remark codes. Remark codes show denial details but are not present for all denials.
The Denials report and the Is Denial? report filter will also now include adjustment codes that indicate denials, even if the entire claim was not denied or there was a partial denial.
Dashboard
- New and Updated Dashboard Gadgets: We are continuing to update the metrics available on your Dashboards. Three new updates were released this week!
- Claim Rejections: This dashboard gadget has been fully reworked to show rejections by the amount of the rejection. The gadget also supports showing payer rejections as well as your claim acceptance rate.
- Claim Denials: This new dashboard gadget will show you the denials that are having the biggest impact on your performance and, therefore, are the first to target to improve your cash flow and revenue cycle management. The gadget also calculates your denial rate, the percentage of your billed claim amounts that are being denied.
- Clean Claims Rate: This new dashboard gadget shows you the percentage of your claim submissions that were accepted by both the clearinghouse and the payer with no rejections. A high clean claim rate means that you’re avoiding issues that prevent payment and require issuing corrected claims.
With these new metrics, you can now add deep insights into your billing performance to your main dashboard!
New Features and Updates
General
Dashboard
- New Dashboard Gadget: Gross Collection Rate: A new dashboard gadget is now available in the Dashboard section, Gross Collection Rate.
Your gross collection rate indicates how well your fees are matched to your allowed amounts. A very low gross collection rate may indicate that your fee schedule amounts are higher than necessary, leading to large adjustments. A very high gross collection rate may indicate that your fee schedule amounts are too low, potentially leading to reduced reimbursements.
Please Note: To ensure that all users have access to this valuable information, and to allow all users to view data for all time, the data for Gross Collection Rate is updated once per day. Changes made during the day will not reflect on this gadget until the next day.
Payment
- Provider Adjustments on ERA: Provider adjustments -- such as Interest, recoupments, and transaction fees -- are available on ERA payments applied from now on. Previously these amounts would show as Unapplied Amounts on ERAs and insurance checks. Now these amounts will show under a separate total and will be reportable as separate positive or negative deposits on, for example, the Daily Deposit report.
Additionally, certain types of provider adjustments, like Interest amounts, will automatically create a Claim Note indicating the amount of interest associated with that claim. Users can also manually link provider-level adjustments to claims to have the system create these notes.
Dashboard
- Procedure Frequency: By Unit Count: Our Procedure Frequency dashboard gadget has been updated with a new display mode: By Unit Count. With this selection, you can now see procedure frequency by the total number of times the procedure was performed, even if the procedure was performed for multiple units.
New Features and Updates
General
Dashboard
- A/R Aging with Amount Over 90 Days Old: The A/R Aging dashboard gadget has been updated to include a new metric: Amount Over 90 Days, which shows the amount and percentage of your A/R that is over 90 days old. You can alternatively report the amount over 120 days if you prefer that metric.
The percentage of A/R that is over 90 days old is an important metric of your practice's performance. Typically, less than around 22% of your A/R should be over 90 days old. If the percentage over 90 days is more than 22%, there may be opportunities for improvement by taking advantage of Eligibility to reduce insurance delays, Electronic Statements and Prompt Payment Discounts to help your patients pay faster, and A/R Control to write off bad debt.
Please Note: To ensure that all users have access to this valuable information, the data for A/R Aging is updated once per day. Changes made during the day will not reflect on this gadget until the next day.
New Features and Updates
General
Dashboard
- New Dashboard Gadget: Days in A/R: A new dashboard gadget is now available in the Dashboard section, Days in A/R.
Days in A/R shows the average number of days that it takes your practice to receive reimbursement, a crucial measure of your revenue cycle performance. Between 35 and 50 represents a healthy practice. A higher than 50 indicates that there are opportunities for improvement.
To ensure that this metric is available for all users, Days in A/R updates its underlying data once per day. Days in A/R will be made available on the Welcome page in a future release.
New Features and Updates
General
Claim
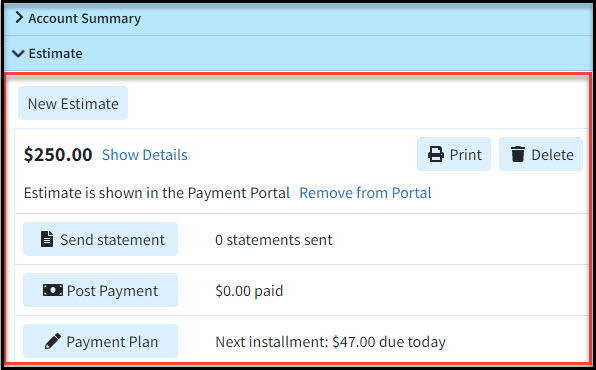
- Estimates are Easier than Ever: You can now use the Quick Estimate feature to allow your patients to pay their Copay online prior to their visit, even if you don't use the Contracts feature, as long as you're set up with our Payment Portal.
We have also removed the need to set up Contracts to create automatic or custom estimates. The system will now estimate the appropriate allowable automatically based on previous payments if there's no contract.
We're continuing to improve our Patient Estimates feature to make complying with the federal No Surprises Act and meeting your patients' needs easier than ever!
New Features and Updates
General
Patient
- International Addresses: Do you ever have patients who are international travelers? CollaborateMD now supports the entry of international or foreign addresses in select areas of the application:
- Patient
- Insured
- Emergency Contact
- Guarantor
- Ambulance Pick-Up Address
These addresses can be submitted on electronic claims, user-printed statements (automated statements are not supported at this time), labels, and more!
New Features and Updates
General
Security
- Per-Customer Roles for Billing Services: If you work in a Billing Service account, you can now restrict Permission Roles to be specific to a single customer rather than working for all customers in your account. When a Role is customer-specific, it can only be applied to a user's permissions in the selected customer.
Admins that only have access to one customer will only be able to create Permission Roles that are specific to their customer. Admins with access to multiple customers will be able to choose which customer each Role applies to. Only Admins and Authorized Representatives with access to every customer within the Billing Service will be able to create or edit Roles that are visible in the entire account.
New Features and Updates
General
Patient
- Apply Copay to Different Dates of Service: When a copay is collected for one date of service but needs to be applied to a different date of service, it's now easier than ever -- the Apply Credit option in Manage Account will now ask you if you want to apply it to other charges if there are no charges for the selected date of service.
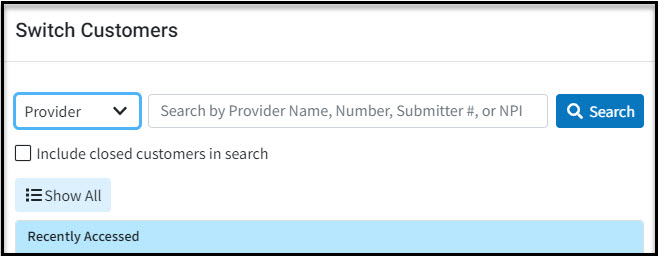
Switch Customers
- Switch Customers by NPI: If you're working your Payer Agreements as a Billing Service, we've added a new convenience feature for you! When you select Provider or Practice as the search option in Switch Customers, you can enter the NPI into the search field to be brought directly to the right customer.
New Features and Updates
General
Payment
- Patient Directed Payment Plans: Save time and get paid faster by letting your patients set up their own Payment Plan from within the Payment Portal!
Set up exactly which patients can set up their own Payment Plans by setting the minimum and maximum balance, payment amount, and term. Then, patients who qualify will automatically see a range of possible payments and can set up a payment plan with automatic payments in minutes, ensuring that you get paid quickly and consistently.
Important Note: You must have the In-App Credit Card Processing and the Patient Payment Portal features enabled and configured in order to use the Patient Directed Payment Plans. Patients setting up payment plans from the portal will be prompted to set up Auto-Pay for their installments in order to complete the payment plan.
Statements
- QR Code on Enhanced Patient Statement: If you have the Payment Portal set up, Enhanced Statements will now include a personalized QR code that takes patients directly to their personalized sign-in page on the portal.

Note: To use enhanced statements you must enable the Enhanced Statements feature for your account, which includes full-color statements, the ability to review past statements in Statement Tracker, and customizable messages throughout the statement!
New Features and Updates
General
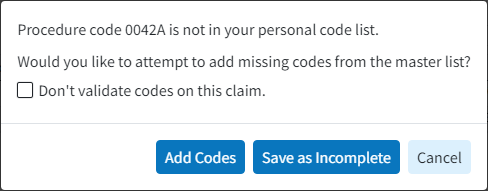
Claim
- Add CPT Codes not in your Local List Automatically from a Claim: Added a new Update to the application so that when saving a Claim that has a CPT code that isn't in your local list, CollaborateMD will now offer to automatically copy that code from the CPT Master List. This eliminates any additional steps involved in manually adding the code to your personal list. The codes contained in the Master List are managed by the American Medical Association (AMA) so you can be confident that the codes will be imported correctly.
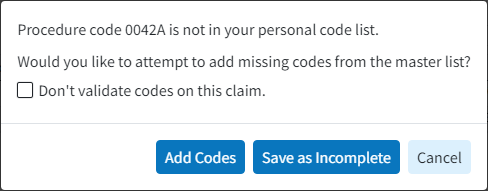
 This applies when new claims are entered manually and when a new claim is created from any Interface (WebAPI, PracticeFusion, etc.), CollaborateMD can now automatically add any CPT codes from the master list that aren't already in your local list.
This applies when new claims are entered manually and when a new claim is created from any Interface (WebAPI, PracticeFusion, etc.), CollaborateMD can now automatically add any CPT codes from the master list that aren't already in your local list.
User Profile
- Added New Password Requirements: Added new password requirements as part of our efforts to continuously improve our security and keep your patients' data safe. Our password requirements have been updated to require that users meet all four of the following complexity rules the next time they change their password:
- At least 1 uppercase character (A-Z)
- At least 1 lowercase character (a-z)
- At least 1 digit (0-9)
- At least 1 special character (punctuation, symbol, or space)
New Features and Updates
General
Customer Setup
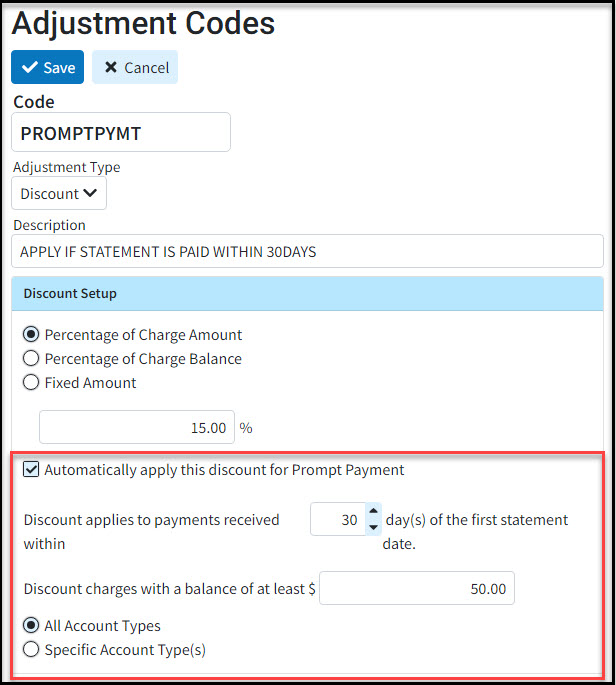
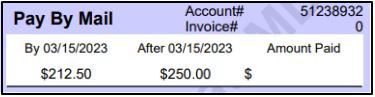
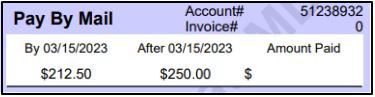
- New Prompt Payment Discount Feature: Added a new patient "Prompt Payment Discount" feature to the application. This feature allows customers to set up a discount code that automatically applies if patients pay within a certain timeframe after their first statement (electronic or paper) is sent. A prompt payment discount will encourage patients to make payments quicker since it will be at a discounted rate if made within the preset timeframe. This reduces the chances of needing to send additional statements, call the patient, or even send the debt to collections.
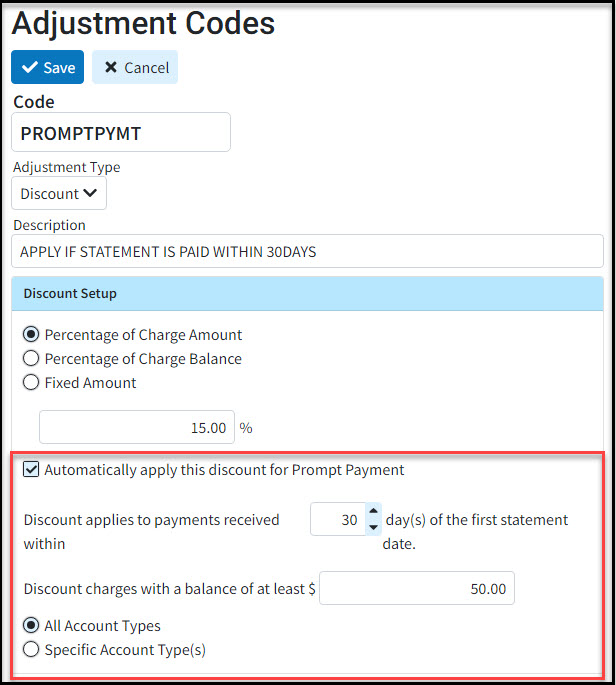
 Patients will see information about the Prompt Payment Discount within the Payment Portal, emailed statements, and paper statements (automatic and user-print). It will show them the amount due with and without the discount.
Patients will see information about the Prompt Payment Discount within the Payment Portal, emailed statements, and paper statements (automatic and user-print). It will show them the amount due with and without the discount.
New Features and Updates
General
Appointment/Claim
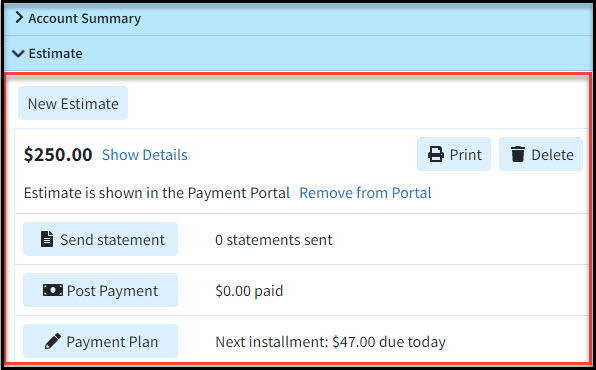
- New Estimates Feature: Added a new patient "Estimates" feature to the application. This feature allows you to easily create accurate Good Faith Estimates from an Appointment or a Claim as required by the No Surprises Act. Providers and billers can now create estimates of patient responsibility at the time of service for uninsured, self-pay patients, or high deductibles and copays. Estimates can be created based on a patient's copay or using the Auto Estimate feature, which generates an estimate based on plan details from the patient's insurance carrier's Eligibility system. Once an estimate is created, users can print the estimate, send a statement, collect payments in the patient payment portal, create payment plans for the estimate, and much more.
Minor Changes and Bug Fixes
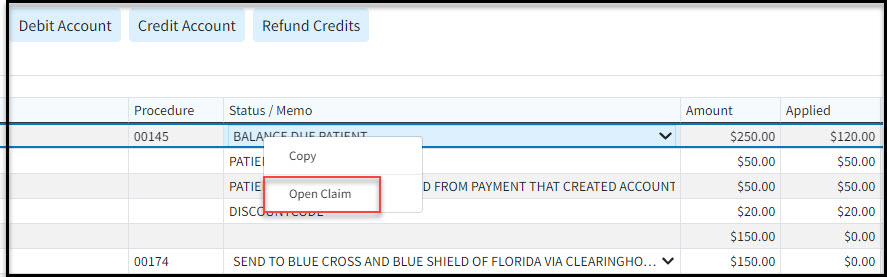
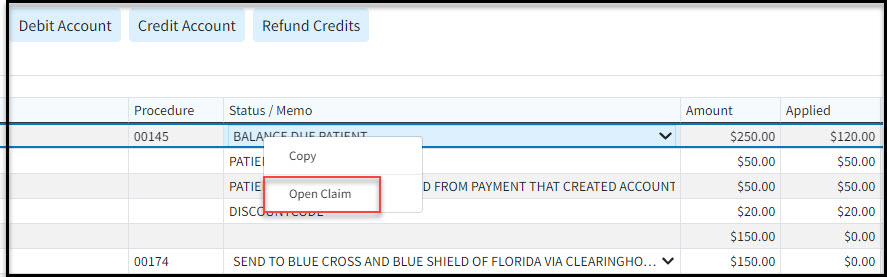
Patient
- Manage Account Right-Click shortcut: Added new right-click options within Manage Account that allow users to open a claim or insurance payment from within the transactions listing table.
New Features and Updates
General
Patient
- New Shortcuts in Manage Account: In Manage Account, a new right-click (long press for touchscreen users) menu has been added. When you right-click on a Claim or Charge, you will have the option to Open Claim. When you right-click on a Payment or Adjustment, you will have the option to Open Payment.
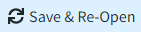 button within Manage Account now allows you to save your changes and automatically close and reopen the screen loading the same patient record. This allows the user to create a credit/debit or action and then immediately act on that item without having to manually reopen the patient record.
button within Manage Account now allows you to save your changes and automatically close and reopen the screen loading the same patient record. This allows the user to create a credit/debit or action and then immediately act on that item without having to manually reopen the patient record.
 This applies when new claims are entered manually and when a new claim is created from any Interface (WebAPI, PracticeFusion, etc.), CollaborateMD can now automatically add any CPT codes from the master list that aren't already in your local list.
This applies when new claims are entered manually and when a new claim is created from any Interface (WebAPI, PracticeFusion, etc.), CollaborateMD can now automatically add any CPT codes from the master list that aren't already in your local list.